
موقع د. كمال سيد الدراوي
طبي_ اكاديمي _ ثقافي _ تعليمي _ _ استشارات طبية_فيديو طبي
|
|
| | Doppler US |  |
| | |
| كاتب الموضوع | رسالة |
|---|
د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: principle of US imaging موضوع: principle of US imaging  الجمعة مايو 31, 2024 7:52 pm الجمعة مايو 31, 2024 7:52 pm | |
|
عدل سابقا من قبل د.كمال سيد في الأربعاء يونيو 05, 2024 9:38 am عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: US probe maneuvers to improve needle and target visualization موضوع: US probe maneuvers to improve needle and target visualization  السبت يونيو 01, 2024 12:37 pm السبت يونيو 01, 2024 12:37 pm | |
| | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Ultrasound Probe Movements and Manipulation موضوع: Ultrasound Probe Movements and Manipulation  السبت يونيو 01, 2024 12:41 pm السبت يونيو 01, 2024 12:41 pm | |
| | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Doppler physics موضوع: Doppler physics  السبت يونيو 01, 2024 4:56 pm السبت يونيو 01, 2024 4:56 pm | |
| Doppler Physics
Dr. Ahmed Abdalrahim Mohamed Ibrahim
FRSMI/AAU
Introduction/doppler effecrt/doppler equation/doppler instrumentation/Color doppler
INTRODUCTION
A good doppler image is based on a good grey scale image showing a range of brightness from very bright to grey to black which is visible as a scale on the L of the screen
In grey scale, the returning echo is assessed by US machine for :
1/ Amplitude {strength} of the echo to get the degree of brightness range i.e a strong echo produces a very bright image; medium level echos result in a grey image; if no echo {echo-free/anechoic}, image will be black
2/ Go-Return time is also assessed by the US machine. The machine will translate time data into distance on the display screen to determine the depth of the structure {echo location}; echoes start from the skin layer, muscles, etc thereby a grey scale image is formed & displayed on the screen.
you see very bright areas, coming from vessels walls, because they are specular reflectors. Black areas represent blood {fluids produce no echoes, i.e all us passes through & no echoes to return to TXR}
3/ in Doppler US the machine assesses a 3RD parameter which is the Echoe's frequency, because US strikes a moving structures i.e the RBCs, & that results in the frequency shift, leading to formation of the doppler image {CD, PWD, CWD, PD}
There will be change {SHIFT or difference} between the transmitted frequency {from probe} & the Recieved frequency {from the RBCs} by the probe.
This change (Shift) in frequency is assessed by the machine to form the doppler image.
within a color box within the display in the form of a color or pulse waveforms or in shape of a graph
Doppler Effect
Is a wave phenomenon in which there is a change in frequency & wavelength due to motion between the source of the wave & the receiver. The receiver is Blood {RBCs} which is moving EITHER towards OR away from the Probe.
There is a change (DUE TO MOTION) b/w Transmitted Frequency of the of the US from the probe striking moving RBCs & the Received Frequency of the echo returning from the moving RBCs.
This difference & change in frequency & wavelength causes different colors (as Christean Doppler stated, after HE observed the different moving colors of the stars at night) christean Doppler stated that when stars are moving down towrds the earth, there will be compression of the wave length (wavelength becomes shorter) & appear BLUE,; & when stars travel upwards towards the sky, there will be rarefaction (elongation of the wavelength & emits a RED color)
1/ IF the Source & Receiver are moving towards each other, the Received wave (ECHO) will have a HIGHER FREQUENCY & a SHORTER WAVELENGTH (compressed) & vice versa
Wavelength or spatial period of a wave or periodic function is the distance over which the wave's shape repeats. In other words, it is the distance between consecutive corresponding points of the same phase on the wave, such as two adjacent crests, troughs, or zero crossings (i.e distance b/w 2 peaks of a WAVE )
When a car is moving towards me (standing waiting), it's sound becomes more louder as it approaches & vice versa. When, the car comes by my side opposite to me I hear no sound because the wavelength is equal in all directions & no change in frequency
SO When blood is moving towards the probe, wave length is shortened (due to rarefaction), & the frequency increases, giving a red color
SO in US, the moving source is blood, & the receiver is the probe ; therefore echo received returning from the moving blood towards the probe will have a higher frequency, SO :
The doppler shift frequency (Doppler shift) is the difference b/w the Received & Transmitted US frequency : Fd = Fr - Ft {doppler sift (Fd) equals Received frequency (Fr) minus Transmitted frequency (Ft)}
When blood flow is towards the TXR, frequency is higher, while wavelength is shorter, & vice versa.
Therefore, Frequecy shift will be positive when the received frequency is higher than the transmitted frequency.
A positive Doppler shit occurs when :
1/ Blood flow is towards the TXR
2/ Received frequency is greater than the Transmitted frequency
A positive dopper shift image is assessed by the machine (subtracts received from transmitted frequency), & is translated as a doppler image & shown as a color or graph on the display
A negative doppler shift occurs when :
1/ Received frequency is less than the Transmitted frequency
2/ Blood flow is away from TXR
A Zero doppler shift occurs when :
1/ Received frequency equals Transmitted frequency
2/ US strikes a stationary object
In this case the machine will collect this Zero difference & displays it on the screen as NO doppler signal i.e NO color
e.g in vascular occlusion (thombosed vein), a vein will show NO color, indicating a non moile thromus
N.B : the symbols, +VE & -VE indicate only direction not magnitude (size/strength) of the shift
NOTE the direction of blood flow in the arteries & veins in the circulation, is opposite to each other. Therefore each will show by a different color on doppler image.
An occluded vessel will show NO doppler signal. | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Doppler Equation موضوع: Doppler Equation  الأحد يونيو 02, 2024 7:12 pm الأحد يونيو 02, 2024 7:12 pm | |
| Doppler Physics
Dr. Ahmed Abdalraheem Mohamed Ibrahim
FRSMI/AAU
Introduction/doppler effect/doppler equation/doppler instrumentation/Color doppler
Doppler Equation
Doppler equation clearly identifies all the factors (4 factors) that affect the magnitude {size/strength} of the doppler shift.
Fd = 2.Ft.V(cos 0)/C
Fd {dopp shift}/Ft {transmitted frequency}/V {Velocity of blood}
cos 0 {cosine theta = angle b/w blood vessel & probe beam direction}
C {US speed}
SO, doppler frequency shift is directly proportional to (the Transmitted Frequency, blood Velocity & cosine theta) BUT Inversely proportional to Speed of sound (which is luckily constant at 1540 m/s); that is to say,1/increasing Ft (transmitted frequency) will increase the Fd (doppler shift)2/increased blood velocity will increase the doppler shift (Fd)
3/ Doppler shift (Fd) is directly proportional to cosine theta, BUT (Fd) will be inversely proportional to the angle theta,which is the angle of insonation b/w the beam direction of TXR & blood vessel (blood flow)
4/ Doppler shift (Fd) will equal to zero (no color signal), when the angle of insonation is 90 degrees i,e perpendicular to the vessel i.e cosine theta will be zero (SO always pay attention to your technical setting).
5/ Doppler shift will be zero when the blood velocity is zero i.e blood is not moving which occurs when vessel is occluded e.g by thromus.
6/ When doppler shift is increased or decreased or zero, the doppler signal appearance on the display will be different
7/ Of the 4 factors which affect the magnitude of the doppler shift : A/the transmitted frequency is constant from the probe B/the the speed of sound is constant at 1540 m/s, therefore the most important two factors which are variable, are the velocity of the blood & the angle.
Once the angle is operator dependent, technical adjusment is easy, guaranteed & tenor by the operator.
The sound of a moving car towards a stationery man will get louder & louder as it approaches him.
When the car reaches him at the very point facing him, there will be NO sound to be heared by the stationary man for a fraction of a second (which is indistinguishable). This is because the angle of insonation of the sound is perpendicular to the stationary man leading to N0 doppler shift
The Angle zero has the highest cosine, 1
The angle 90 degrees has the least cosine, 0 i.e at RT angles (perpendicular), the doppler shift is zero leading to No doppler signal on the display {multiplying zero by the doppler equation results in zero}.
The angle 60 degrees has a cosine of 0.5
Scanning with different angles in the same pt in the same time, will result in different doppler shifts.
When scanning with angle near 90 degrees, the graf of the pulse wave will go below the baseline.
The color inside the color box is a doppler shift
steering the color box is a maneuver to adjust (change) insonating angle.
when adjusing (steering) color box in different angles results in different doppler shifts (color strength) from strong to weak color, & to No color at all if angle of insonation (b/w US beam & vessel) is steered (adjusted) perpendicular at 90 degrees.
Several stages for image formation till display
1. Received returning US echo signal from body tissue is sent into the Central Prossessing Unit (CPU) of the of the machine
is sent into the echo image prossesor room which will result in the ordinary grey scale US.
2. Then is sent into doppler area to the doppler direction detector.
3. Then sent into the doppler velocity estimator.
4. Thereby, doppler image is formed & displayed on the screen.
عدل سابقا من قبل د.كمال سيد في الأربعاء يونيو 05, 2024 9:37 am عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: رد: Doppler US موضوع: رد: Doppler US  الإثنين يونيو 03, 2024 7:02 pm الإثنين يونيو 03, 2024 7:02 pm | |
| Doppler Physics
Dr. Ahmed Abdalrahim Mohamed Ibrahim
FRSMI/AAU
Introduction
doppler effect/doppler equation/doppler instrumentation/Color doppler
Doppler Instrumentation
Types of Doppler Instruments
1.Continuous Wave Doppler {CWD} in echocardiography
2. Pulsed Wave Doppler {PWD} gives graphical display
3. Color Flow Doppler/Color Flow Imaging/Color Doppler Imaging {CD} gives Red
4. Color Power Imaging {PD} gives ONE color, but recently there is PD with directional Angio.
Power Doppler, is a mapping of power to a continuous color range, is compared to color flow imaging. The direction and Doppler velocity are encoded as a dual display in which colors represent velocities in terms of the Doppler spectrum and also the direction of flow to and from the transducer.
The blood flow information is obtained in Three different ways {all three are doppler shifts} :
1. Audible sound (artery sound can be distinguished from sound of the vein) N.B : Here we hear the shift frequency which is in the audible range, NOT the US, because US is inaudible to human hearing
2. spectral display
3. color flow image
The factors which can change the color or the graph or the sound, are those of the doppler shift equation.
The changes, from low to high to NO color of the 3 shifts in the display are all controlled by the 4 factors of the doppler equation: Transmitted frequency, blood velocity, The angle (cosine theta), & speed of sound.
Any change in these factors will change the shap or quality of these doppler shifts (color, graf, or sound)
the change in the shits will be A/from deep red to light or blue color B/the spectral graph may be higher, lower, or below the baseline C/ Loud or quiete sound
IF doppler shift is zero, there will be NO color , NO graph, NO sound
IF shift is increased, the deep red color will be light red, the graph amplitude will be higher, the sound will be louder.
IF shift is decreased, the color will be deep red, graph amplitude will decrease, sound will be quiet
As stated earlier, that the transmitted frequency and the angle & the sound speed are all constant, Therefore the only variable that cause shift changes is the blood velovity.
IN spectral doppler the dopp shift information is depicted in a waveform.
IN color doppler, the dopp shift information is utilized to show the blood flow in color
Different doppler systems
Duples systems
Are US scanners that provide TWO capabilities : A/ Greyscale B- mode imaging B/ Spectral Display
Triplex systemsAre US systems that provide THREE capabilities :
A/ greyscale B-mode imagingB/ color flow and/or color power imagingC/ spectral display Directional or Bidirectional instruments These are capable of A/ distinguishing b/w +Ve & -Ve Doppler shifts AND B/ presenting the signals in separate channels for hearing or viewing Directional or (Bidirectional) instrument means :1. can provide flow direction, i.e can 2. differentiate b/w negative & positive shifts, i.e can 3. differntiate b/w vein & arteryUnidirectional instrumentsThese cannot differentiate b/w negative & positive dopp shifts, like Power Doppler US systems (give same color to both arteries & veins)
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Color Doppler موضوع: Color Doppler  الأربعاء يونيو 05, 2024 2:27 pm الأربعاء يونيو 05, 2024 2:27 pm | |
| Color Doppler
Is used to :
1/To evaluate a relatively large area for the presence & direction of blood flow, e.g is it a vein or artery (i.e is it a positive or a negative doppler shift)
2/ To rapidly detect the doppler shifts over the large area within the color box; most color systems use a technique called Autocorrelation to detect the doppler shifts.
3/ Higher magnitude doppler shifts are diplayed in LIGHTER shades of the assign color.
4/ (It is controlled by velocity changes) Fow velocities are usually indicated by color brightness. Usually, the flow in the center of the blood vessel is very fast with higher frequency doppler shift, while slow in the periphery of the vessel due the friction of the blood with the wall of the vessel, thus leading to lower doppler shift frequency in the vessel periphery; Therefor we have different colors of the blood within the vessel: dark in the periphery; & light shade of brightness in the center; that is because the doppler shift has faster velocity in the center leading to higher doppler shift frequency in the center of the flow.IF velocity is abnormally increased, Artifact will occur called {Aliasing}
Color Doppler InstrumentationThe most important are : 1/ the color box : A/ which is a region on the display within which doppler information (the doppler sfift){i.e the colors in the color box} is displayed. B/ The shape of the color box differs with the type of the probe used : 1. With convex probe, the shape of color box will be Trapezoid With 2. linear probe, the shape of the color box will be Rectangular.C/ The color box has a setting & under the control of operator & can be adjusted increasing or decreasing 2/ The color Maps : A/ determine which colors are assigned to the detected doppler shift B/ TWO types of doppler maps 1. color Bar (most commonly used) A/ with TOW channels, separated in the middle by Black Bar as Baseline, with the positive shift in the upper OR lower part (assigned as Red color or blue 2. color wheel 3/ variance Maps :B/ there is always color gradient in the color Bar; when gradient from dark blue (low +v shift) to light blue (high +v shift) & vice versa; & the same applies to to the color box.
IF velocity is abnormally increased, Artifact will occur called {Aliasing}:IF a shift exceeds the Nyquist limit it is mapped with a LIGHTER shade from the the opposite channel, & this is called ALIASING.The Nyquist limit is the maximum limit the US machine can display the doppler shift without artifact.When the shift abnormally exceeds the upper limit, {Nyquist limit}, that the machine can detect the shift, there will be mixing of color (light shades from one channel adjacent to light shades from the opposite channel, i.e color mixing) & called aliasing & always occurs in the center of blood vessel & with light shades. It usually occurs in cases of stenosis (where velocity is zero i.e blood is not moving i.e NO flow, which leads to higher flow velocities, leading to higher doppler shift frequencies, (shifts increase from the middle of the color Bar upward & downward), & when velocity becomes abnormally high exceeding the nyquist limit, mixing of colors occurs i,e ALIASING) which is a powerful tool in the investigation of stenotic vascular coditions.
In cases of Flow reversal it is different from Aliasing in that there are (dark shades of blue from one channel adjacent to black & dark shades of red from the opposite channel), which leads to change (Reverse) the flow directionVariance MapsIs a 1. specialized form of color map that 2. can display one additional piece of information 3. In addition to the TWO main colors used for the positive & negative doppler shifts, the varance map displays a third Green color (which is used to indicate turbulence) beside the red & blue colors. to 4. indicate the locations in the cplor box from which a wide range of doppler shifts are being detected 5. Can be used anywhere in the body, BUT mainly used in pediatric echocardiography for diagnosing congenital defects, e.g VDS, ASD etc.. to show the Turbulent flow, which is the most common cause of a wide degree of variance in the detected doppler shifts. 6. Variance maps should NOT be confused with RainBow maps which contain SOME geen adjacent to the blue color. These maps are commonly used in vascular scanning
7. With RainBow maps, the green A/ does not indicate turbulence, but merely B/ helps to differentiate levels of doppler frequency shifts in the negative direction Color ControlsAs stated earlier, to aquire a good doppler image, yu should obtain a good greyscale image first. Therefore, good knowledge of Knobology & controls is essential. A/ Primary CD controls
1. (optimum selection) Transducer
2. Application Preset Menue (AP) is a basic important First step. Press to select organ of interest, & the whole set of the organ will be selected automatically, (probe,frequency,etc...)
3. Output power 4.Image Depth (+ve/-ve zoom) 5. (perform steering in case of linear probe) Color box Angle 6. Color Box Width can be adjusted increasing or decreasing, BUT if width is increased too much, will affect the Frame Rate
7. Color Gain (usually start with high Gain setting, if searching for presence or absence of flow), then gradually decrease the gain
8. Scale (PRF) (Velocity Scale)
9. Invert control :To change the setting of the color BAR by depicting (the +ve shift as blue instead of red & vice versa)
B/ Secondary CD controls 1. Wall Filter 2. Doppler frequency 3. Packet Size 4. Echo-write priority 5. Baseline
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Color Controls موضوع: Color Controls  الخميس يونيو 06, 2024 7:18 pm الخميس يونيو 06, 2024 7:18 pm | |
| DOPPLER PHYSICS contdDr. Ahmed AbdAlranim
Color Controls contdAs stated earlier, to aquire a good doppler image, yu should obtain a good greyscale image by good background of physics, proper machine setting understanding of controls & knobology A/ Primary CD controls Controls & settings are frequently adjusted to obtain a good image 1. Transducer : 1/Appropriate probe selection for appropriate exam (correct TXR & correct frequency). 2/ Same probe used for greyscale, will be used for doppler scanning. 3/ For peripheral vascular & superficial studies, Rectangular high frequency linear array probes are used, while a wide bandwidth convex array probe is used for deep abdomen, pelvic & obgyn studies. 4/ that is due to compromise b/w Resolution & Penetration 2. Application Preset Menue (AP) 1/1ST step is to select the type of exam from the menu e.g, carotid & automatically 2/the name of the exam selected will appear on the screen, & 3/all the setting of the machine will be carotid. 4/It will select a rectangular linear high frequency probe, the PRF, & all carotid measurements. 3.Output power
Always 1/ keep the power as it is, OR keep the power at the Lowest level
Try to 2/ implement the ALARA principle {As Low As Reasonably Acheivable}
To 3/ obtain good doppler signals, it may be necessary to use a little more power than with corresponding greyscale image.3/ As doppler intensity is higher than greyscale, especially in PWD, always great caution is required when using doppler in early pregnancy & sensitive organs e.g testes, {Therefore it is prudent to use less power when scanning sensitive tissue. 4/Always monitor MI {Mechanical index} & TI {Thermal index} on the screen 4.Image Depth (+ve/-ve zoom) 1/ Use the shallowest depth setting that will allow allow yu to image the ROI 2/ Excessive depth :A/increases the PRP [Pulse Repetition Period],B/wastes time, C/ and Reduce Frame rate D/ keep it shallow & zoom it up 5. Color box Angle The Color box 1/ can be steered to RT & LT oR straight.
2/ A Rectangular linear array TXR forms a rectangular color box.
3/ The rectangle can be steered to the RT or LT to form a parallelogram4/ By this technique of Steering (control knob),we are changing the doppler angle : when steering straight, the angle b/w the beam & vessel, (optimum doppler angle is b/w 60 & 45 degrees), will be perpendicular (90 degrees), & the doppler shift will be zero & no color is displayed (because cosine 90 is zero) due to incorrect technical setting
5/ A linear array TXR steers the beam for color doppler in the same way as Phased array TXR, which steers it's beam electronically by the technique of firing the active elements with very slight time delays, causing the beam to veer off at an angle from the TXR face.
6/ If the electric cuurent is sent at the same time the crystal elements will fire at the same time without delays leading to a straight beam (Not to the RT or to the LT)7/ Every probe has a different shape of color box than other probes; SO the color doppler image shows variation in the displayed color throughout the length of the tube, with NO color at 90 degrees8/ Convex probe forms a Trapezoid beam (color box) & the whole box can be moved around the screen from side to side ;BUT cannot be steered like linear, because it's beam is sent at different angles, leading to different colors due to variation in the transmitted beam angles, giving red & blue but NO color when angle is 90 degrees
9/ The PD shows little variation in the displayed color except for 90 degrees10/ When a vessel is tortuous , will give different colors , from red to blue according to its direction of low (towards or away from the probe) 11/ Often, by moving the box, & by angling the TXR, yu will be able to obtain a good doppler angle
12/ In a convex TXR, the scan lines are not parallel, SO yu will be obtaining a range of doppler shifts(& thus a range of colors) due to the variety of angles.6. Color Box Width Width 1/ can be adjusted increasing or decreasing, BUT wider color boxes contain more color lines {scan lines} leading to decreased Frame Rate & a slow image formation, SO it is better to keep it small. 2/ Usually, frame rate is not a problem in superficial structures, but it matters with deep structures, when we should reduce the color box width when possible so as to increase the frame rate, e.g in Obgyn & abdomen 7. Color Gain Always 1/start with higher Gain setting, if mainly searching for presence or absence of flow, then gradually reduce gain as appropriate. 2/ The knob nominated as CF in the controls A/when pressed, it shows color B/when rotated, it denotes gain increase or reduce 3/ Set A/Higher gain till many colors occur on the display (called Noise).B/Then reduce Gain gradually till color just reaches the intimal surfae of the blood vessel i.e doppler shift is seen inside the vessels {Color within the blood vessels & NOT outside the bloold vessel} 4/ When color Gain is too low, trickle flow (very small flow, will not be seen) may go undetected, thus missing an important information. 5/ When color gain is excessive & higher than optimal, the color will exceed the limits of the artery & there will be bleeding {bleed out} i.e color outside the blood vessel into the wall & surrounding tissues, thus limiting visualization of important pathology like thrombus (plaque surface)
6/ Every type of doppler system has a different type of gain, & appears as a percentage on the display 8. Scale (PRF) (Velocity Scale)
1/ There is a knob named scale & sometimes named PRF, which can be moved up & down to a miximum of 60
2/ The scale controls the PRF
3/ PRF determines Nyquist limit {the maximum doppler shift the machine can detet without Aliasing artifact occurs} 4/ Increasing the scale will increase the Nyquist limit & vice versa5/ The scale is set So that normal blood flow produces doppler signal shifts which are just below the nyquist limitwhen exam of interest is correctly selected from the preset application the machine will automatically select the whole correct data needed for the exam e.g correct (probe, frequency,measuremesnts, scale etc.
6/ If scale is set below the mean velocity of the blood flow (adjusted very narrow), Aliasing will occur throughout the vessel lumen even in the normal blood flow; because by reducing the scale (PRF), the nyquist limit (maximum limit) will also be reduced so that alasing occurs even in normal blood flow 7/ IF scale is significantly set the higher than the mean velocity of the blood flow (very wide scale), aliasing may disappear but will result in a missed stenosis (stenosis will be missed due to the very wide scale) [very important information at 51 mins & 30 sec of 2nd video doppler physics dr. ahmed abd alrahim] 8/ Abnormally fast flowing blood (increased velocity) will then produce a high doppler frequency shift (Fd) that exceeds the nyquist limit. These shift will Alias & will be immediately recognizable on the display 9/ Any A/Aliasing seen indicates an increase in doppler shift which will be caused by one or more of the factors of the doppler equation. B/AS stated before, the Ft
and speed of sound, are constant; the angle theta is correctly adjusted by operator, it will be the blood velocity that has increased. C/ The velocity is always very high in the area of stenosis leading to increased doppler shift which will cause focal aliasing. D/ Aliasing will not be visible when scale setting is too high already far above the nyquist limit E/ the area of aliasing indictes the area of vessel stenosis, & the thrombus will be seen as a hyperechoic area F/ Aliasing will involve the whole vessel if the scale is reduced (very narrow) G/ the correct setting is to adjust gain & scale so that *the doppler shift (color signal) is within the vessel *and blood in the center of the vessel is light red, & at the periphery dark red. 9. Invert control Allows operator to 1/ invert the colors in the +ve & -Ve channels on the color map in the color Bar. That is by assigning the blue color as positive instead of the conventional red, & vice versa 2/ Invert is post processing, & the change can be done later after images are saved.
عدل سابقا من قبل د.كمال سيد في السبت يونيو 08, 2024 7:17 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Secondary CD controls موضوع: Secondary CD controls  السبت يونيو 08, 2024 7:13 pm السبت يونيو 08, 2024 7:13 pm | |
| DOPPLER PHYSICS contd
Dr. Ahmed AbdAlranim
Color Controls contd
B/ Secondary CD controls
1. Wall Filter
1/ In doppler US, any motion detected will produce a doppler signale.g bowel gas, respiration, etc
2/ A knob under operator control, It is filtering (Rejecting) high amplitude low frequency shifts that come from the movement of the vessel wall rather than the movement of the blood.
3/ The baseline (the black line) b/w the +v & -ve channels, is the indicator of wall filter in
the screen
4/ On some systems, the position of the wall filter is indicated by the thickness of the color baseline ; while on other systems additional indicators are placed on the color map.
5/ A thick baseline indicates a high baseline, which appears as an incomplete filling of the vessel (low flow & not good fill in) leading to missing of some of the doppler information
6/ For venous studies, wall filter is better kept off or very low, since there is little wall motion
2. Doppler frequency
Basically (by default), Doppler frequency is automatically set by the machine to a level 1/ lower than greyscale to insure better penetration.
2/ But for deeper studies, the TXR's doppler transmit frequency will be set by the application preset selected for the study
3/ The doppler frequency control (knob) can allow the sonographer to slightly increase or decrease the doppler transmit frequency which, depending on the situation, may improve the color display
3. Packet Size
1/ In CD, the packet size {Pulse packet, ensemble length} is the number of pulses sent down each scan line to detect doppler shifts
2/ The A/number of pulses per line is termed {ensemble length, packet size, shots per line, or pulse-listen cycles per acoustic scan lines}. B/The number of pulses transmitted in one second is the pulse repetition frequency (PRF). C/ How many of those pulses are fired on each scan line is the ensemble length.
D/The range is 3 to 32 with a default of around(10)
3/ Increasing the packet size A/will increase the number of pulses sent down each scan line & B/should improve the detection of doppler shifts ; C/this is useful in situations where it is critically important to increase the packet size to increase the sensitivity of doppler to detect small flow, there by to be able to determine the presence or absence of flow (e.g testicular tortion)
4/ The negative aspect of increasing the packet size (increased number of pulses per scan line), is the corresponding reduction of frame rate
5/ The US image A/ is known as a frame. B/ Multiple frames produced in rapid succession form the moving or real-time image we see on the ultrasound monitor. C/ Frame rates in modern systems are typically 10 – 30 frames per second and a D/a flicker free image is achieved using electronic smoothing techniques
4. Echo-write priority
1/ "Also known as "Echo vs Color Threshold" or just "Color Priority
2/ This control allows sonographer to determine whether a pixel will display color information or greyscale information
3/ The threshold {cut- off point} can be set by sonographer based on echo amplitude
4/ Echoes with amplitudes above the threshold value will only be displayed in greyscale.
5/ Echoes with amplitudes below the threshold will be displayed in color if they have a doppler shift
6/ This knob is usually constant & is not changed or adjusted by sonogapher
5. Baseline
1/ Is an important control because it is the division b/w the positive & the negative channels
2/ It is usually indicated on the color map by a BLACK BAR of variable width
3/ By default, the system preset usually sets the baseline to the center b/w the two channels.
4/ The baseline control allows the Sonographer to shift the baseline up or down which will increase the scale in one channel at the expense of the other.
5/ On some systems A/the displayed width of the baseline (thick black bar vs thin black Bar) is used to indicate the wall filter threshold B/{The wall filter is indicated by the thickness of the baseline} C/ the thickness of the baseline indicates wall filter setting, i.e
High wall filter indicates thicker black bar baseline, while very low wall filter indicates a thin black bar baseline
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: رد: Doppler US موضوع: رد: Doppler US  الإثنين يونيو 10, 2024 2:43 pm الإثنين يونيو 10, 2024 2:43 pm | |
| DOPPLER PHYSICS contd
Dr. Ahmed AbdAlranim
Color doppler contd
Display of doppler information
The two basic doppler data displayed as color pixel in color flow imaging (CFI) are
1/ The Reflector direction
A/ which will differentiate b/w +ve & -ve doppler shifts, & B/ differentiating b/w vein & artery, as (they are* flowing in opposite directions,* each with a different color from the other)
2/ The Average reflector {blood} velocity
Average, (i.e NOT the accurate blood flow velocity), because A/Color doppler detects Only presence or absence of flow B/In CD, blood velocity information is given in color & NOT in quantitative digits e.g C/ increased velocity increases the doppler shift which is indicated by lighter shade of red color & vice versa
D/ Accurate Blood velocity information is calculated by the PWD, & not color doppler
To detect presence or absence of flow
* Anticipate the type of flow yu are looking for from menu Application preset, then set the CD controls appropriately at the start
* Low velocity flow (especially the angle not close to zero degrees), will require sensitive settings
* SO optimize yr primary controls to detect low amplitude shifts
* Try to obtain a good doppler angle
* If flow is not detected, examine another region of tissue in which yu know there is flow
this is critically important in e.g testicluar torsion (No flow indicates definitely torsion)
* One should be able to tell the direction of flow when using color doppler
* Normal or abnormal flow is governed by TXR location & the anatomy
To assess flow direction
1. Look at the color in the vessel, is it red or blue
2. Relate the color to the color map & what does it indicate a +ve or a -ve shift
3. Determine the relationship of the blood flow to the TXR (the angle of the color box to the vessel will tell yu the location pf the TXR)
4. Knowing the location of the TXR & the shift, yu should be able to determine the flow direction
عدل سابقا من قبل د.كمال سيد في الثلاثاء يونيو 11, 2024 8:55 am عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Doppler Artefacts موضوع: Doppler Artefacts  الإثنين يونيو 10, 2024 7:15 pm الإثنين يونيو 10, 2024 7:15 pm | |
|
DOPPLER PHYSICS contd
Dr. Ahmed AbdAlranim
Color doppler contd
Doppler Artefacts
Causes, appearance, avoidance
Some artifacts are useful & beneficial to doppler image, others cause image disturbance.
Causes of artefacts are due to
1. Technical limitations & machine setting e.g A/too high Gain setting will lead to color bleed out i.e color outside the vessel lumen). B/IF wall filter is set too high we miss a lot of important doppler information needed
thus losing good fill in
C/ very narrow scale causes Aliasing
2. * Due to pt anatomy : e.g flash artefact due to motion coming from the heart OR mirror artefact due to specular reflector like the diaphragm.
3. Due to machine factor : like winkle artefact when US vibration in the stone causes mixed of red & blue color posterior to the stone called twinkle artefact.
1/ Aliasing Artifact
* Is a doppler artifact that ca occur in both CD & PWD
* Occurs when the detected doppler shift exceeds the upper limit (Nyquist limit) that the system can accurately detect without causing artifact (called aliasing)
* Blood Velocity, almost always is the main factor which is increased dramatically in stenotic vascular disease, because the other factors of the doppler equation are not affeccted
*Aliased signals are mapped in the light shades of color from the opposit channel
2/ Mirror Artifact
* There must be a specular reflector same as in greyscale for Mirror artifact to occur e.g liver mass appears on both sides of diaphragm & lung area. Also in carotid scan it is called carotid ghost
* It is got rid off by changing the angle
* Occurs when there is turbulence flow which leads to post stenosis A/tissue vibration, B/pressure fluctuations,C/ vessel wall vibrations & D/ perivascular tissue vibration
* Blood is normally flowing, then sudden stenotic area leads to turbulence after stenosis with blood flowing in all directions
3/ Flash artefact
* Is typically a high-amplitude, BUT low frequency shift signal
* :The concept of physics include
A/ Motion of pt body B/ Motion of the probe C/ Motion of any anatomic structure secondary to an external force e.g during LT lobe of the liver scanning, flash artefact occurs due to extensive motion from the heart
* Can be suppressed, minimized & reduced by using the {Motion (Noise) Discriminator Function}, which can be found in most machines
* Can be reduced on the display, BY increasing the wall filter, but important information about slow flow can be missed
* Flash artefact mainly preferentially dominates hypoechic areas, causing color within fluid-filled structures e.g GB & cysts, etc
* & As stated earlier,A/ doppler is very sensitive to motion, B/ even probe motion, respiration, bowel motion, all cause disturbance & noise.C/ Advantages & useful information we get from flash artefacts in: @ the UB, where flash artefact in urine jet, informs about patency of ureter. @ Blood motion
Urine D/ jet is due to high velocity of urine when entering the UB (small ureteric orifice)
4/ Twinkle artefact
* There is mixed of color posterior to a stone instead of posterior shadowing
* Physics A/concept : US is pressure waves which causes vibration. when vibration occurs in the stone, Twinkle artefact can result posterior to the stone
B/ Advantages & useful informations we get from twinkle artefact: @when a small stone could not be seen in greyscale, then put color, & twinkle artefact in the urine jet which indicates the presence of small stone & which also diagnosis a patent ureter
@ When a small ureteric stone is impacted in the VUJ, & the shadow is not visible in greyscale, we put doppler & there appears the twinkle artefact (which is mixing in colors posterior to a the stone)
5/ Dirty shadow Artefact
Occurs A/mainly due to gas, B/ ring down artifact due to bubble movement | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: CD advantages vs disadvantages موضوع: CD advantages vs disadvantages  الثلاثاء يونيو 11, 2024 9:26 pm الثلاثاء يونيو 11, 2024 9:26 pm | |
| DOPPLER PHYSICS contd
Dr. Ahmed AbdAlranim
Color doppler contd
CD advantages
Its ability to quickly assess a realtively large area for the Presence & Direction of flow i.e A/determines whether vein or artery (+VE "towards" or -VE "away from" probe
B/e.g ovarian or testicular torsion (flow= "OK" or NO flow= "Torsion") C/ hypoechoic hepatic mass (is it solid mass or abscess; putting color shows color & direction of flow CD disadvantages
1. Displays the average doppler shifts (velocity information displayed as color (NOT the peak accurate numerical value)
2. Semiquantitative & gives no numerical values
3. It's detrimental effect on the Frame Rate (FR), which is low in CD
4. CD is Angle dependent (probe at 90 degree yields zero doppler shift)
5. Aliasing (No aliasing in CWD)
6. Artefacts caused by the noise (due to motion, because CD is very sensitive to the least motion even probe motion results in a doppler shift)
7. CD has Poor temporal resolution (Resolution related to time) resulting in very low FR
Color Doppler Conclusion
Good CD can usually be obtained :
1. With the use of the correct preset application
2. A Good understanding of doppler principles
3. Appropriate adjustment of the primary color controls
4. Secondary controls may also be adjusted in order to optimize the color display
عدل سابقا من قبل د.كمال سيد في الأربعاء يونيو 12, 2024 4:40 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: CD Qs & As موضوع: CD Qs & As  الأربعاء يونيو 12, 2024 1:28 pm الأربعاء يونيو 12, 2024 1:28 pm | |
| Color Doppler Qs & As
1. ?packet size in CD refers to the number of:
a/ pulses per second b/ sample volumes per scan line c/ scan lines per unit area
d/ pulse/listen cycles per acoustic scan line e/ pulses required to create one frame
2. greatest doppler shift is obtained when angle is zero & highest velocity (diagram)
3. What method is used to steer the color beam with linear array TXR?
a/ mechanical b/ electronic time delays c/ electronic time variation d/ Apodization e/ the color beam cannot be steered with a linear array TXR
electronic time delays are automatically set by the machine*
* Apodization is one of the most widely used methods for reducing side lobes in an ultrasound focusing system. This method reduces side lobe levels by multiplying signals in the transmit and receive channels by weights, but decreases the resolution by increasing the main lobe width.
4. yu obtaind a CD image of the CCA .If the received US frequency is greater than the transmitted US frequency. which of the following would be correct ?
a/ color encoded red -ve doppler shift b/ color encoded blue -ve doppler shift c/ color encoded red +ve doppler shift d/ color encoded blue +ve doppler shift e/ no doppler shift was detected
* there are three possibilities for any doppler shift, either +v or -ve or zero doppler shift
* Fr greater than Ft : A/indicates +ve shift with B/flow towards TXR & C/appears above the baseline in the color map D/BY default the +ve shift is set as red
* Fr equals Ft frequency, doppler shift equal zero
5. ?increasing wall filter during doppler sampling will :
a/ increase visibility of low fequency signals b/ increase spectral broadening c/ decrease bandwidth d/ reduce display of low frequency shifts e/ reduce aliasing
* the indicator of the wall filter in the screen is the thickness of the baseline
* wall filter has no relation with aliasing
* increasing the wall filter will (filter) reduce the display of low frequency shifts (which come from the movements of the arterial wall)
6. what would be the most likely result from increasing transmit frequency of the CD ?
a/improved sensitivity to slow flow b/improved penetration for imaging blood flow in deeper tissues
c/ reduce flash artifact obscuring small vessel flow d/ reduced CD aliasing e/ improved visibility of complex flow hemodynamics
* It is opposite to aliasing (d), aliasing is caused by increased frequency which leads to increased doppler shift
* flash artefact (c) is reduced by A/ noise reduction B/wall filter
* to image deeper tissues (b) yu have to reduce frequency not to increase it
* increasing frequency (a) will increase the sensitivity of CD to detect slow flow
* there is an option in the preset application menu to increase or decrease the transmitted txr frequency
7. ?doppler frequency shift is defined as :
a/ the difference b/w doppler frequency & the imaging frequency b/ the difference b/w transmitted & received frequency c/ the time b/w the transmitted & received pulses d/ the rate at which the TXR emits pulses e/ the amplitude of the transmitted doppler signal
* imaging frequency (a) means greyscale
* doppler frequency shift is neither Time (c) NOR Rate (d)
* doppler frequency shift is NOT an amplitude
* doppler shift frequency is the differenceb/w Ft & Fr
8. According to the doppler equation, which of the following is NOT true?
a/ increasing doppler frequency will increase the frequency shift b/ increasing the doppler interrogation angle will increase the frequency shift c/ decreasing the reflector speed will decrease the frequency shift d/ NO frequency shift is detected when the doppler beam strikes the reflector with perpendicular incidence e/ velocity information can can be obtained from the frequency shift if the angle of incidence is known
* doppler shift is directly proportional to the transmitted frequency, velocity, & cosine theta, BUT inversely proprtional to the angle theta (b is the incorrect answer)
9. Nyquist limit describes which of the following?
a/ penetration limit of PWD b/ transit time of PWD c/ sampling frequency needed for detecting the doppler signal unambiguously d/ sampling method used for CWD e/ method used for determining directional information in a doppler shifted signal
* Nyquist limit has NO relation with penetration (a) OR time (b) OR direction (e)
* unambiguously (c) means correctly, without artefact
10. during abdominal doppler scan yu adjusted several system controls & noticed that the FR has decreased. which of the following adjustments would yu perform to improve the color frame rate?
a/ increase packet size b/ decrease the PRF c/ decrease the color box width d/ increase the scan line density
e/ increase the wall filter
* frame rate A/ is mostly affected by the color box width B/ wider color box width means much more scan lines, resulting in decreased frame rate C/ always keep color box width small (c)
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: CD Qs & As موضوع: CD Qs & As  الخميس يونيو 13, 2024 7:13 pm الخميس يونيو 13, 2024 7:13 pm | |
| CD Qs & As contd
11/ The rapid technique used in most CD systems to obtain the mean doppler frequency shift is ?
a/ fast fourier transform b/ phase quadrature c/ autocorrelation d/ zero-crossing detector e/ variance
There is a software in the machine (electronic circuit) named autocorrletion which determines the frequency shift*
*Autocorrelation is the most common method used to estimate velocity in color flow imaging.
Measurement of reflector velocity is obtained by manipulating the echo-induced signals gener- ated from consecutive transmitted pulses.
12/ What term describes the number of pules that are used to determine the velocity along a color line of sight?
a/ color gate b/ packet size c/ PRF d/ pulse duration e/ pulse repetition period
13/ what display method will help yu to demonstrate flow turbulence with CD?
a/ autocorrelation b/ variance c/ fast fourier analysis d/ zero-crossing detection e/ pulse quadrature detection
It is the map variance (b) in which the green color helps to determine turbulence
14/ Color flash artefact is obscuring the anatomy of interest in an exam of the abdominal Aorta
?what can yu do to reduce impact of the flash
* there are two methods to reduce flash artefact
a/ increase the color gain b/ decrease the PRF c/ increase the wall filter
d/ decrease the packet size e/ increase the doppler transmit frequency
the 1st method is to apply the noise (motion) reduction*
* (c) the second method is to increase the wall filter
15/ While evaluating the liver vasculature with color doppler, yu are unable to obtain signals from the deeper vessels.
What should yu do to enhance yur ability to demonstrate deep flow?
a/ decrease the packet size b/ increase the scan line density c/increase the wall filterd
d/ increase the PRF e/decrease the US frequency
* deeper vessels need more penetration, & achieved by reducing US frequency (e)
16/ Which of the following statements about formation of CD image is TRUE?
a/ the color & B-Mode images are generally derived from the same pulse
b/ the color image is superimposed on the the existing B-Mode image
c/ the color & B-Mode images are generally formed using the same frequency sound wave
d/ the B-Mode image is usually obtained at a lower frequency than the color image
e/ the color image generally has a higher spatial resolution compared to the B-Mode image.
17/ Which of the following actions would decrease CD Frame Rate
a/decreasing frequency b/increasing line density c/decreasing packet size
d/decreasing color box size e/increasing gain
* Decreasing color box size (d) will increase Frame rate
* Increasing scan line density {by increasing the color box size} will decrease the Frame Rate
* line density is the number of scan lines
18/ What is the result of increasing the wall filter during doppler sampling?
a/increased visibility of low-velocity signals b/increased spectral broadening c/decreased bandwidth
d/reduced display of low-velocity doppler signals e/reduction of aliasing
* increasing wall filter will result in Reduction of display of low-frequency doppler signals (d)\
19/ If yu increase the doppler transmit frequency which of the following will result?
a/velocity will increase b/doppler frequency shift will increase c/penetration will increase
d/the frame rate will increase e/the nyquist limit will increase
* According to the doppler equation, increasing any factor (EXCEPT speed pf sound),will increase the doppler frequency shift
20/ which control optimization should yu make to improve CD sensitivity to slow flow?
a/lower packet size b/lower the transmitted US frequency c/Raise the PRF
d/lower the wall filter setting e/lower the threshold
As stated earlier, increasing wall filter will dismiss & remove (filter) all the slow flow signals*
* therefore to make sure that the slow flow is present, try to reduce wall filter setting (d) as much as possible
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: رد: Doppler US موضوع: رد: Doppler US  الأربعاء يونيو 19, 2024 7:40 pm الأربعاء يونيو 19, 2024 7:40 pm | |
| Doppler physics (Pulsed Wave Doppler) PWD
Prof Ahmed Arahim
1/ PWD is a form of spectral doppler (Graphical display), the doppler shift is displayed as a graph
2/ PWD is a graphical display of the detected doppler shift spectrum (the range of doppler shifts) from the flowing blood.
3/ In PWD the variation in doppler shift is marked by variation in magnitude of the graph spike height; higher spike indicates higher doppler shifts
4/ THUS PWD privides most detail about blood flow
CD : 1.provides A/Presence or absence of flow B/Direction of flow 2.CD shift is displayed as color 3. the variation in CD shift is marked by variation in color, being light "when high shift" & dark shade "when low shift
5/ PWD is applied after: 1ST good greyscale image & see vessels. 2ND put color doppler to the greyscale image to detect blood flow. 3RD apply the PWD for more details
e.g velocity, flow characteristics, etc
6/ Only the doppler shifts from within the sample volume, are evaluated, giving PWD excellent range resolution. PWD only measures velocity at a single point in the sample gate (Sample volume), which is a great advantage of PWD /7
8/ Positive shifts (arteries) are displayed above the baseline, while negative shits (veins) are displayed below the baseline
9/ When blood flow is towards the probe, the graph will be above the baseline (Upward signal=+ve shift),while we get a (Downward signal = -ve shift) when blood flow is away from the probe
10/ The sample volume should Not be longer than one third of the vessel diameter size
A small (narrow) sample volume size results in a Narrow graph display, while a wide sample volume gives a wide graph display
11/ Using a larger sample volume 1.will capture the slower flow velocities that occur near the vessel walls
in addition to 2.the higher velocities from the vessel center. 3. This leads to variation in velocities which results in variations in doppler shifts 4. and the graph will be thick 5. So a large gate (sample volume) is used when searching only for flow
12/ Using a narrow sample volume 1.will capture only the fastest flow in the vessel center resulting in narrow graphical display 2.So smaller gate is used to detect precise information e.g calculating the PSV
3. The position of the sample volume should be in the center of the blood vessel
13/ : Important notifications
1. The intensity of PWD tends to be significantly higher than the intensity of either CD or greyscale imaging
2. PWD uses longer pulses AND higher PRFs than are used for imaging
3. The following US imaging modes are presented in order of increasing heating potential
A/ Greyscale B-Mode
B/ Harmonic imaging
C/ M-Mode
D/ CD
E/ PWD
4. Therefore, PWD should be used wit great caution especially in sensitive organs, e.g early pregnancy unless clinically indicated
PWD instrumentation
1/ TXR
* PWD uses the same probe used in greyscale imaging linear, curvilinear, phased array,TVS, or All-In-One Handheld etc
* For organ of interest selected from preset application, the appropriate probe is selected automatically by the machine
* Similar to CD, PWD tends to transmit at a slightly lower frequency than the corresponding imaging frequency to insure for better penetration
* probe is connected to the Pulser (in the CPU) which emits electrical pulses to activate the PZE crystals
* Then probe sends the pulse & receive back the echoes into the Receiver which contains the quadrature detector which calculates the doppler shift (Fr minus Ft)
* The information is then displayed into the loud speaker compartment to form a sound
* Then is sent to the spectrum analyzer to form the spectral display
* Then the information is displayed on the screen monitor | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: PWD instrumentation contd موضوع: PWD instrumentation contd  السبت يونيو 22, 2024 1:04 pm السبت يونيو 22, 2024 1:04 pm | |
| PWD contd
PWD instrumentation contd
2/ Receiver
.1 Electronically, the position & the size of sample volume, are controlled by the receiver
2. In PWD A/ the receiver is GATED, i.e reads information from a certain gate. B/The gate is the area of the sample volume, which opens & closes (send impulses, then off then receive, & so on). C/ This means that the receiver will only process echoes for doppler shifts that arrive when the gate is open
3. Gating provides PWD with one of it's biggest (greatest) advantages, namely excellent range resolution because it reads the information from the sample volume
3/ Quadrature Phase Detector (QPD)
1.Is the fancy physics term for the electronic circuits in the receiver that actually detect the doppler shift
2. It does this just as we would expect : by electronically subtracting the Received from the transmitted frequency. & The difference b/w the two is the doppler shift frequency, which is within the audible range (that is why we hear the sound of the blood flow in artery different from that of the vein).
3. Increased or decreased volume of the sound implies a an increase or decrease in the doppler shift.
4.Then information displayed into the loud speaker room, & then displayed on the monitor screen
5. As These doppler shifts are audible we can hear them, & with practice can make sence of them e.g normal or stenotic etc .So always keep the loudspeaker open during scanning
6. Higher frequency shifts will have a higher pitch (pitch is frequency) there fore the pitch of the vein is lower than artery pitch due to lower vein shift
4/ Spectrum analyzer
1. This component A/interrogates the complex doppler shift signal & B/determines every frequency it contains & C/the strength of those frequencies D/ & it does this 50 times/sec by using a computer process called a Fast Fourier Transform (FFT)
2. The FFT processor A/analyzes the contents of any type of doppler shift variation (for single frequency) & B/displays it in a dotted graf form inside the system. C/then it is demodulated & displayed as a graphical representation of analyzed doppler shifts in its final shape on the monitor .
3. The spectral display, displays three components of the doppler shift as they occur over time :
A/ The Shift direction, (blood flow direction of the shift), & when it is towards the probe, it will be displayed above the baseline & implies a positive shift
* The baseline, on the spectral display, is represented by a black bar on the color map on the RT top of the screen. It separates the positive (channel "shift") from the negative (channel "shift")
B/ The Shift magnitude, (Is Size of the doppler shift) i.e refer to the two primary doppler equation parameters which affect the magnitude of the doppler shift : i.e @ Blood velocity @ Doppler angle
* Higher shifts are displayed farther from the baseline i.e tall spikes up the graph
* Lower shifts are displayed closer to the baseline i.e short upward spikes
N.B :
(IN color doppler, higher shifts are displayed as lighter shades of red, while lower shifts appear darker color*)
C/ The Shift amplitude, (is the strength of the shift; like the degree of brightness in greyscale) i.e wheather a strong or a weak signal
Factors affecting the shift amplitude signal :
* Out put power: increasing the output power will increase the brightness
* Attenuation
* Acoustic impedance mismatch (Echo intensity): the greater the mismatch, the stronger the echo
* Type of reflector e.g specular reflector increases amplitude
* Gain: increasing the gain increases the degree of brightness
@ In the spectral display, the amplitude of the doppler shift is represented on the Z-axis by the brightness of the display
@ The brighter the spectral display, the higher the amplitude (strength) of the
doppler shift
@ Strong shifts are displayed with bright pixels
@ Weaker shifts are displayed by darker pixels
Fundamental features of the spectral display
1. Time: is displayed in the horizontal axis (x-axis)
2. (Y-axis) Shift magnitude: is displayed on the vertical axis
3. Shift amplitude: is represented on the Z-axis (the degree of brightness "echo srength")
@ The baseline separates the positive (above the baseline) from the negative channels (shifts) below the baseline.
4. Window: is the clear empty area located underneath the spectrum b/w the graph & the baseline & is called the spectral window.
*when the window (empty space) is filled in, is called spectral broadening
* The received doppler shift consists of a range of frequencies
* Narrow range of frequencies will result in a narrow display line
5. Nyquist limit: *is the maximum doppler shift that is displayed by the doppler machine correctly without any aliasing. *It is the upper limit of each channel. *It can be changed by changing the scale
عدل سابقا من قبل د.كمال سيد في الإثنين يوليو 15, 2024 11:39 am عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: PWD controls موضوع: PWD controls  الأحد يوليو 14, 2024 7:28 pm الأحد يوليو 14, 2024 7:28 pm | |
| PWD contd
Pulsed Wave Dopller Controls
Primary PWD controls
1. TXR selection
2. Preset
3. output power
4. image depth (+/- zoom)
5. doppler angle
6. sample volume position
7. PW doppler gain
8. baseline
9. doppler scale (in khz=Fd, or cm/sec, m/s=blood velocity)
10. ( invert/ inverted- & +) invert control
11. angle correction
12. measurement calipers
1/ Spectral doppler Gain
* It amplifies the strength of the doppler signals
* Start with higher gain setting then reduce the gain as appropriate
* Too high gain will produce background noise
2/ Baseline
* It is adjusted frequently by shifting it upwards or downwards
* It divides the spectral display into positive & negative channels
* It controls the PRF
* .(Nyquist limit = PRF/2) The PRF determines the Nyquist limit
* increasing the scale, increases the Nyquist limit & vice versa
* Baseline can be displayed in kHz (doppler shift)or cm/sec or m/s (blood velocity)
* The vertical axis either displays doppler shift in kHz OR can be made to display blood velocity in cm/sec or in m/sec
3/ Angle correction
#IF the spectral waveform is only being assessed for the direction of flow, presence or absence of flow, or the character of flow (arterial vs venous), angle correction is NOT needed
# IF the velocity scale is being used & blood velocity is being used to make diagnostic decisions (e.g PSV in carotid stenosis), then accurate Angle correction is critical because the decision of stenosis depends on blood velocity .
#when angle correction key is set, a small cursor appears within the sample volume & it usually alligned parallel to the walls of the vessel
# Without angle correction the system will always assume a doppler angle of zero degrees & this will overestimate the true blood velocity because cosine zero is one which is the highest velocity
# The purpose of angle correction is to provide the US system with the correct doppler angle b/w the blood flow & the TXR, then the system uses the angle to accurately calculate the blood velocity.
# Angle correction is a post proccessing control, i.e yu can re calculate & revise the angle later
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Secondary Doppler Controls موضوع: Secondary Doppler Controls  الثلاثاء يوليو 16, 2024 4:17 pm الثلاثاء يوليو 16, 2024 4:17 pm | |
| PWD contd
Secondary Doppler Controls
1. PWD Wall filter
* Is designed to remove & Reject unwanted low frequency shifts arising from the motion of vessel walls & cardiac chambers
* The thickness of the baseline indicates the wall filter
# REMember/ In Color doppler, there will be NO good filling of the shift in the vessel when wall filter is increased.
*BUT in PWD high wall filter is indicated by a GAP b/w the graph & baseline. this gap indicates the Removal of all the wanted low doppler shifts (both positive & negative) below a certain threshold
* For venous study, always keep wall filter OFF or very low, because wall motion is limited
* when wall filter is set too high (it is numerated) there will be a gap b/w the graph & the baseline
because it will remove & reject all the low doppler shifts (both positive & negative) below a certain threshold
2. PW Doppler frequency
* same as in CD yu can try changing the transmit frequency as appropriate according to pt size etc
3. PWD Sample volume (1 - 15 mm)
* A small sample volume is desirable (One third the diameter of the vessel), as this gives the best axial resolution
* in some cases a larger sample volume is helpful particularly when searching for Elusive flow (difficult to find)
4. Sweep speed
*Is used to adjust the graph speed, fast or low as wanted
* It controls the interval of time that is displayed on the horizontal (X) axis of the spectral display
* Using a fast sweep speed the spectrum can usually only display 1-2 normal cardiac cycles
* decreasing sweep speed will display a longer interval of time (6-8 seconds) & the waveform will scroll by more slowly resulting in displaying 7 or more normal cardiac cycles
# But we usually depend on the default setting of the machine already set
5. Duplex control
* A Doppler machine with capability of displaying greyscale & spectral display
* The greyscale image is frozen while the doppler spectrum is being displayed
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: PWD measurements موضوع: PWD measurements  الثلاثاء يوليو 16, 2024 4:21 pm الثلاثاء يوليو 16, 2024 4:21 pm | |
| PWD contd
measurements that can be made on the spectral display
All measurements are calculated by automeasurement by the US machine
1. PSV
* Peack systolic velocity is a measure of the blood's maximum maximum velocity during systole. (The cardiac cycle consists of sytole, early diastole, & late diastole)
* PSV is measured from the the highest point in the cycle down to the baseline
2. EDV
End Diastoilc Velocity is a measure of the blood's maximum velocity at the end of diastole
3. RI (Pourcelot index)
* Resistive Index : RI = (PSV minus EDV) / PSV
* The range for RI is 0 to 1
* Most arterial waveforms have a RI of less than 0.7
4. PI
* Pulsatility Index performs a similar function to RI
* It is less frequently used
* PI = PSV minus EDV / mean velocity recorded throughout the cardiac cycle
* Most low resisance areterial flow waveforms have a PI of less than 1.8
5. S/D ratio
* Is the systolic diastolic ratio (systoilc velocity/diastolic velocity)
* mostly commonly used in obstetris
* SD = PSV/EDV
6. Acceleration time
7. Acceleration index
8. HR
Spectral doppler Assessment
In PWD yu 1st check for flow :
{1} IF flow is detected, that is ok
{2} IF NO flow detected :
1/ Check machine sensitivity
2/ check sample volume placement
3/ check beam/flow angle
@ IF sensitivity is good, it is ok
@ IF machine sensitivity is decreased, it can be Improved BY :
1. Increasing power or gain, will improve US machine sensitivity to detect the flow
2. Decreasing the velocity scale
3. Dereasing the reject or filter
IF wall filter was set too high, slow flow is rejected & all information will not be detected by the machine
4. slowly increasing the sample volume size
# Aliasing occurs when the doppler shifts exceed the Nyquist limit "wrapped around i.e cut" & the signal will be displayed at the high end o the opposite channel i.e the opposit end of the color map
# Nyquist = PFR/2
# Aliasing will be corrected by moving the baseline downwards
# When aliasing occurs in the stage of Color doppler (before applying PWD), it occurs as mixing of colors (light shades of red with light shades of blue) in a specific focal area of the vessel (area of stenosis). IN this area of stenosis we apply the PWD & take our measurement of the doppler shift. It will show a high doppler shift exceeding the Nyquist limit. For correcting aliasis, Use the baseline knob to move the baseline downwards
Adjustments made to avoid aliasing
1. use baseline knob to move the baseline downwards to show the whole graph
When the scale (PRF) setting is increased, the Nyquist limit is increased, thereby decreasing the likelihood of aliasing.
2. Increase the scale
3. decrease frequency
4. (changing the angle) decreasing doppler shift frequency
By using multiple sample volumes, the pulse repetition frequency (PRF) is increased (the pulses from different sample volumes are added) and thus the aliasing speed is increased. This is referred to as high PRF Doppler or extended range Doppler.
High PRF emits greater energy, essentially because it doesn't wait as long to send out another pulse. Upside of high PRF: Greater energy improves detection at long range.
The PRF is the pulse repetition frequency and determines the sensitivity to slow flow. The PRF must be kept as low as possible (around 500 Hz) because linked with the PRF adjustments are the filters. The higher the PRF the higher the filters are, and high filters will eliminate slow flow.
PRF is normally expressed as the number of pulses transmitted in 1 s and is therefore denoted in Hertz or pps (pulses per second)
With high PRF settings, lower velocity signals are filtered out by the high-pass wall filter resulting in loss of sensitivity to slow flows [27]. ... ... Doppler signal is influenced by multiple physical factors and technical parameters such as Doppler frequency, Pulse repetition frequency and wall filters.
Aliasing artifacts occur when the structure being examined exceeds the maximum velocity set by the Nyquist limit. You can reduce the effects of the artifact by decreasing the transducer's frequency, decreasing depth, and choosing an anatomic structure with a velocity below the Nyquist limit.
عدل سابقا من قبل د.كمال سيد في الإثنين أكتوبر 28, 2024 5:25 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Hemodynamics principles موضوع: Hemodynamics principles  الخميس يوليو 18, 2024 7:53 pm الخميس يوليو 18, 2024 7:53 pm | |
| Hemodynamics principles
Shape of blood flow
Continuous (Laminar) flow parabolic
*As the blood travels inside the vessel for a longer distance, there will be velocity variation
* Blood velocity in the center of the flow is usually faster the the in the periphery.
*It is slower in the periphery due to the presence of the vessel walls resistance.
* Therefor there will be lighter color in the center, & a darker color in the periphery
* Laminar flow is characterized by constant velocity over time
* Flow profile is determined by inertial & frictional forces with faster velocity towards the center & decreased velocity at the vessel wall
decreased velocity at the vessel wall
# Transition from laminar to turbulent flow
* Turbulent flow occurs when laminar flow breaks down & particles in the fluid move randomly in all directions with different speeds
* when the range of velocities increases significantly, the flow pattern becomes turbulent
* Reynolds number, describes the point at which flow becomes turbulent
* =Reynolds number Equation :
Average flow speed X Tube diameter X density
* Turbulent flow is characterized by :
1. always occurs after the stenosis
2. the spectral window will be filled in, & called spectral broadening
3. blood moving at different directions
# Non laminar flow / the Flattened flow/ Plug flow
*Blood is moving with the same velocity as it is exiting the heart & in the beginning of the tube (vessel & color is uniform across the vessel
* As blood moves for a longer distance, the variation in velocity occurs, accompanied by color variation
* The empty space b/w the graph & baseline is called Presystolic window
# Pulsatile flow
* Changes periodically over time
* Flow is highly pulsatile in the extremity arteries due to the high peripheral resistance at rest resulting in the typical Triphasic doppler waveform
* low resistance is indicated by an elevated (high) end diastole from the baseline
* As vessel resistance increases, end diastole reaches the baseline & more over descends below the baseline resulting in the triphasic waveform (phase 1, phase 2, phase 3
# High resistance flow
* Reults in a more pulsatile flow with an acceleration phase, followed by deceleration, & a significant reflux below the baseline in early diastole & a short backward flow in mid-diastole
* Zero flow is typically seen in end diastole this pattern is referred to as tri-phasic flow
* High resistance flow is typically of the extremity arteries supplying muscles & skin
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Hemodynamics principles موضوع: Hemodynamics principles  الجمعة يوليو 19, 2024 2:11 pm الجمعة يوليو 19, 2024 2:11 pm | |
| Hemodynamics principles contd
# Low resistance flow
* Arteries supplying parenchymal organs & the brain are characterized by a fairly steady blood flow as a result of low peripheral resistance So, the blood enters the organ without resistance. e.g renal artery
* In these arteries a moderate systolic rise, is followed by a steady forward flow that persists throughout diastole, with NO reflux below the baseline
* The shape of the graph is characterized by A/ a thin systolic rise because all the blood moves with the same velocity, B/ a slightly thicker early diastole, because variation of velocities starts with early diastole C/ & a more thicker late diastole because the variation in velocity becomes larger D/ the whole spectral graph above the baseline
# High resistance vs Low resistance waveforms
* The difference b/w the two is most evident in diastole
1. vessels that supply blood to high resistance arteriolar bed, display reduced forward flow velocity in diastole, & may even demonstrate reversed flow in early diastole
2. vessels supplying low-resistance arteriolar bed, will display good forward velocities throughout systole & diastole with a high end diastole from the baseline
# Doppler Spectrum Assessment
Blood flow can either be :
1. Mono-phasic
2. Bi-phasic
3. Tri-phasic
4. Bi-directional
@ IN Mono-phasic flow, the whole graph is above the baseline i.e flow is just on one side of the baseline.
@ IN Bi-phasic flow, the blood flow starts on one side above the baseline, & then crosses to the other side below the baseline
@ The Tri-phasic flow starts on one side above the baseline with forward flow in systole, then crosses to the other side below the baseline as diastolic flow reversal, then returns to the original side above the baseline with forward flow in late diastole examples are femoral artery, popliteal artery, anterior tibial artery, posterior tibial artery; all are tri-phasic with high resistance flow
@ Bi-directional flow, is a blood flow which occurs simultaneousely on both sides, above & below the baseline at the same time
# Spectral window
* A narrow range of frequencies results in a large clear spectral window
* Spectral window is an empty space b/w the arterial signal & the baseline with absence of doppler signal below the spectrum
* example; large superficial arteries, femoral, carotids
# Spectral broadening (Window fill-in)
* Is a wider range of frequency shifts at any given point in time that causes a FILL-IN of the spectral window
* this occurs :
1. after stenosis
2. high doppler gain
3. high power settings
4. large sample volumes
5. small vessels
@ There will be no empty space
@ It occurs in stenosis due to variations in directions & velocities of blood flow & with turbulence
@ A large sample volume means taking a range of velocities from center & peripheral of the vessel flow resulting in spectral broadening (FILL-IN)
@In small vessels like renal, testicular, hepatic & uterine arteries, the sample volume cannot be placed in the center of the vessel The sample volume will fit the same diameter of the small artery resulting in doppler shift velocity variations which causes the window to be filled in
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Hemodynamics principles موضوع: Hemodynamics principles  السبت يوليو 20, 2024 12:22 pm السبت يوليو 20, 2024 12:22 pm | |
| SPECTRAL ANALYSIS in different arteries
1/ High pulsatility/resistance Tri-phasic waveform
* sharp systolic peak
* reversed diastolic flow
* e.g extremity artery in resting stage
2/ Low pulsatility/resistance waveform
* broad systolic peak
* forward flow in diastole
* e.g ICA, vertebral, renal, celiac
3/ Mixed pulsatility/resistance waveform
* Sharp systolic peak
* Forward flow in diastole
* e.g ECA & SMA during fasting stage
* When the end diastole approaches the baseline, will imply increasing resistance
# Spectral changes in Disturbed flow
1/ (Parabolic) Laminar flow
The normal Laminar flow is characterized by a @ narrow spectral width & a @ clean window
2/ Disturbed (Non-laminar flow)
There is @ spectral broadening resulting in @ loss of the spectral window because blood is flowing with different velocities in different directions
3/ Turbulent flow
* Erratic (irregular) flow
* Spectral broadening
* Loss of spectral window
* Reversed systolic component
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Doppler Flow Imaging and Spectral Analysis موضوع: Doppler Flow Imaging and Spectral Analysis  السبت يوليو 20, 2024 7:37 pm السبت يوليو 20, 2024 7:37 pm | |
| Doppler Flow Imaging and Spectral AnalysisIntroductionIn this chapter, we review the concepts and principles necessary for understanding and interpreting color Doppler images and pulsed Doppler waveforms and discuss the key elements needed for the interpretation of Doppler spectral waveforms. This includes a study of normal waveform patterns and characteristic changes that occur with pathologic states. Important tips are given for recognizing Doppler spectral features that are essential for the diagnosis of arterial stenosis and occlusion. We discuss the principles of color and power Doppler, including the advantages and limitations of these imaging modes. Finally, we conclude with a brief overview of three-dimensional (3D) and B-mode imaging.Blood Flow PatternsIn general, blood vessels change size and direction as they course through the body. Blood flow velocities also change depending on the size of the vessel lumen and the change in direction of flow. In addition, arterial blood flow is pulsatile and faster in the center of the vessel and slower at the periphery of the vessel lumen. Moreover, the vessel lumen may be distorted by atherosclerosis and other pathology. For these reasons, during Doppler evaluation, blood flow produces a mixture of Doppler frequency shifts that changes from moment to moment and from place to place within the vessel lumen. Spectrum analysis is needed to sort out the jumble of Doppler frequencies generated by blood flow and to provide quantitative information that is critical for diagnosis of vascular pathology.The Doppler spectrumThe word spectrum , derived from Latin, means image . You may think of the Doppler spectrum as an image of the Doppler frequencies generated by moving blood. In fact, this image is a graph showing the mixture of Doppler frequencies present in a specified sample of a vessel over a short period of time. The key elements of the Doppler spectrum are time , frequency , velocity , and Doppler signal power; these elements appear on the images presented in Fig. 3.1 . Please refer to the images while reading about these important components of the color and spectral displays. We begin with Fig. 3.1A :
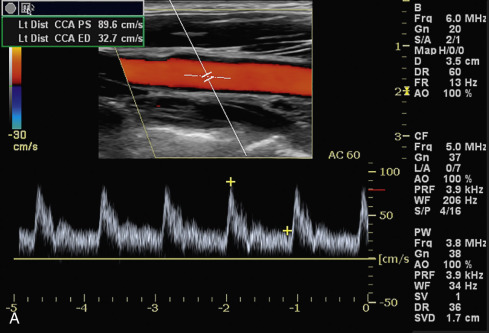 Color flow image: The vessel, the sample volume, and the Doppler angle are shown in the color flow image at the top half of the display screen. Color flow image: The vessel, the sample volume, and the Doppler angle are shown in the color flow image at the top half of the display screen.
Color flow information: The color bar to the left of the image shows the relationship between the direction of blood flow and the colors in the flow image. By convention, the upper half of the bar shows flow toward the transducer. This is logical because this part of the bar is nearest to the transducer in the image. The lower half represents flow away from the transducer. In this case, red/yellow colors correspond to flow toward the transducers, and blue/light blue colors indicate flow in the opposite direction. A shift in color from red to yellow or from blue to light blue represents increasing flow velocity.
Doppler angle: The Doppler angle for the spectral Doppler appears to the right of the color flow image, in this case 60 degrees (AC 60 = angle correction 60 degrees).
Time: The time is represented on the horizontal ( x ) axis of the Doppler spectrum at the base of the display. The lines represent divisions of a second, but a scale is not always provided.
Velocity: Blood flow velocity (cm/s) is shown on the vertical ( y ) axis of the spectrum. In this case, velocity is shown on the vertical axis as cm/s (centimeters/second).
The distribution of velocities within the sample volume is illustrated by the brightness of the spectral display (the z -axis). To better understand the z -axis concept, examine the magnified spectrum shown in (B) and imagine that the spectral display is made of tiny squares called pixels (picture elements). You cannot see the pixels in this image because they are purposely blurred to smooth the picture. The pixels are there, however, and each corresponds to a specific moment in time and a specific frequency shift or velocity. The brightness of a pixel (its z-axis) is proportionate to the number of blood cells causing that frequency shift at that specific point in time . In this example, the pixels at asterisk 1 are bright white, meaning that a large number of blood cells have the corresponding velocity (about 90 cm/s) at that moment in time. The pixels just below asterisk 2 are slightly darker, meaning that fewer blood cells have the corresponding velocity (about 20 cm/s) at that moment. The pixels below asterisk 3 are black, meaning that no (or very few) blood cells have the corresponding velocity at that moment. If this is not clear, read this again and remember that the brightness of each pixel is proportionate to the relative number of blood cells with a specific velocity at a specific moment in time. Because the brightness of the pixels also shows the distribution of flow energy, or power, at each moment in time, the spectrum display is also called a power spectrum.
Flow direction : The direction of flow is shown in relation to the spectrum baseline. In this case, flow toward the transducer is shown above the baseline, and flow away from the transducer is shown below the baseline. Note that the number 50 in the lower right corner is preceded by a minus sign. Because the area below the baseline corresponds to flow away from the transducer, a negative Doppler shift is generated. The relationship between the flow direction and the Doppler baseline may be reversed by the operator, but flow toward the transducer will always be represented by positive velocity or frequency values.
Pulse repetition frequency : Please note the pulse repetition frequency (PRF) on the display on Fig. 3.1A . The PRF for the color flow image is shown on the right of the image under CF (color flow) and is 3.9 kHz. The PRF for the spectral Doppler is located underneath, under PW (pulsed wave) and is also 3.9 kHz. A higher PRF may be needed for the spectral Doppler to ensure that systolic velocities are shown accurately, without aliasing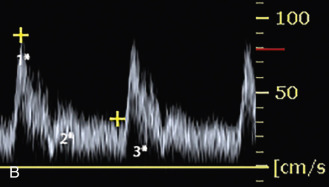 https://radiologykey.com/doppler-flow-imaging-and-spectral-analysis/ https://radiologykey.com/doppler-flow-imaging-and-spectral-analysis/
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: رد: Doppler US موضوع: رد: Doppler US  الأحد يوليو 21, 2024 7:03 pm الأحد يوليو 21, 2024 7:03 pm | |
| What is a power spectrum?
The Doppler frequency spectrum reviewed in Fig. 3.1 is sometimes called a power spectrum because the power, or strength, of each frequency is shown by the brightness of the pixels. The power of a given frequency shift, in turn, is proportionate to the number of red blood cells producing that frequency shift. If a large number of blood cells are moving at the same velocity, the corresponding Doppler frequency shift is powerful, and the pixels assigned to that frequency shift (velocity) are bright. Conversely, if the same number of red blood cells are moving at slightly different velocities then the pixels assigned to the corresponding frequency shifts are dimmer. The power spectrum concept is important for understanding power Doppler flow imaging, which is discussed later in this chapter. The concept of the power Doppler spectrum is nicely illustrated in Fig. 2.35 .Frequency shift conversion to velocity information
The echoes that are reflected back to the transducer from moving cells in a sampled blood vessel contain only Doppler frequency shift information; however, the Doppler spectrum usually displays velocity (cm/s or m/s) information. How does the instrument convert the Doppler frequency shift to velocity? This conversion occurs when the sonographer “informs” the duplex instrument of the Doppler angle, which is shown in Fig. 3.2 . If the instrument “knows” the Doppler angle, it can then compute the blood flow velocity via the Doppler formula (see Chapter 2 ).Note in this equation that the Doppler frequency f D is proportional to the cosine of the Doppler angle theta and the flow velocity. When the operator informs the ultrasound machine of this angle, the Doppler frequency shift becomes a velocity measurement. A Doppler angle of 60 degrees or less is required to derive accurate frequency and velocity measurements. If the angle is greater than 60 degrees, velocity measurements are unreliable. Although there is greater error in measurements obtained at higher angles, some applications (e.g., carotid examinations) are more easily performed at angles closer to 60 degrees. For greatest accuracy, it is generally recommended that the Doppler angle should be less than or equal to, but not greater than, 60 degrees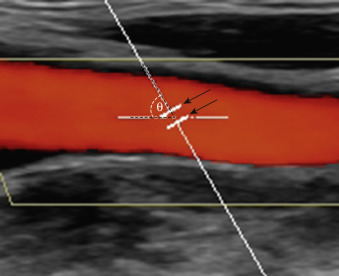 FIG. 3.2The Doppler angle and sample volume. The nearly vertical line is the Doppler line of sight. The line in the center of the blood vessel indicates the axis of blood flow. The angle formed by these two lines is the Doppler angle (θ). The parallel lines ( arrows ) indicate the length of the Doppler sample volume.It is desirable to operate the duplex instrument in the velocity mode rather than the frequency mode for several reasons. First, velocity measurements compensate for variations in vessel alignment relative to the skin surface. For instance, the Doppler frequency shift observed in a tortuous internal carotid artery might be radically different from one point to another, but angle-corrected velocity measurements will be similar throughout the vessel, in spite of dramatic changes in vessel orientation relative to the skin. Second, the Doppler frequency shift is inherently linked to the output frequency of the transducer, but velocity measurement is independent of the transducer frequency. For instance, if the output frequency goes from 5 to 10 MHz, the frequency shift is doubled. This could lead to misinterpretation of the findings. If transducers with different frequencies were used to determine stenosis severity, different diagnostic parameters would be needed for each ultrasound transducer (e.g., 3.5, 5, 7.5 MHz). This problem is eliminated when the instrument converts the raw frequency information to velocity data. Third, current diagnostic criteria are presented as velocity parameters. Frequency information is no longer used to determine severity of disease. Practical TipsThe key elements of the Doppler spectrum are time , frequency , velocity , and Doppler signal power .By convention, the upper half of the color bar and the upper part of the Doppler spectral display show blood flow directed toward the transducer.A Doppler angle of 60 degrees or less is required to derive accurate frequency and velocity measurements. The Doppler angle should always be checked when using velocity information. FIG. 3.2The Doppler angle and sample volume. The nearly vertical line is the Doppler line of sight. The line in the center of the blood vessel indicates the axis of blood flow. The angle formed by these two lines is the Doppler angle (θ). The parallel lines ( arrows ) indicate the length of the Doppler sample volume.It is desirable to operate the duplex instrument in the velocity mode rather than the frequency mode for several reasons. First, velocity measurements compensate for variations in vessel alignment relative to the skin surface. For instance, the Doppler frequency shift observed in a tortuous internal carotid artery might be radically different from one point to another, but angle-corrected velocity measurements will be similar throughout the vessel, in spite of dramatic changes in vessel orientation relative to the skin. Second, the Doppler frequency shift is inherently linked to the output frequency of the transducer, but velocity measurement is independent of the transducer frequency. For instance, if the output frequency goes from 5 to 10 MHz, the frequency shift is doubled. This could lead to misinterpretation of the findings. If transducers with different frequencies were used to determine stenosis severity, different diagnostic parameters would be needed for each ultrasound transducer (e.g., 3.5, 5, 7.5 MHz). This problem is eliminated when the instrument converts the raw frequency information to velocity data. Third, current diagnostic criteria are presented as velocity parameters. Frequency information is no longer used to determine severity of disease. Practical TipsThe key elements of the Doppler spectrum are time , frequency , velocity , and Doppler signal power .By convention, the upper half of the color bar and the upper part of the Doppler spectral display show blood flow directed toward the transducer.A Doppler angle of 60 degrees or less is required to derive accurate frequency and velocity measurements. The Doppler angle should always be checked when using velocity information.
Listening to the Auditory Frequency SpectrumThe human ear was the instrument used initially for Doppler blood flow studies. The ear is a highly capable spectrum analysis instrument, which is evident in its ability to distinguish one person’s voice from another. Even though duplex ultrasound instruments are equipped with electronic spectrum analysis devices, an audible Doppler output is provided as well, to take advantage of the human ear’s capabilities. Certain features of the Doppler flow signal can be appreciated aurally that are difficult or impossible to display electronically, and as a result, the audible Doppler signal remains important in ultrasound vascular diagnosis. For instance, in very high-grade carotid stenoses, a distinctive high-pitched whining or whistling sound is heard. In spite of its abilities, however, the human ear has three major drawbacks. First, the ear is a purely qualitative device; second, it is not equipped with a hard copy output for permanent storage; and third, some ears work better than others—some cannot hear very high frequencies. Electronic spectrum analysis overcomes these obstacles.https://radiologykey.com/doppler-flow-imaging-and-spectral-analysis/
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: رد: Doppler US موضوع: رد: Doppler US  الأحد يوليو 21, 2024 7:54 pm الأحد يوليو 21, 2024 7:54 pm | |
| The sample volumeThe frequency spectrum displays blood flow information from a specific location called the Doppler sample volume , illustrated in Fig. 3.2 . You should be familiar with the following three characteristics of the Doppler sample volume: First, it is, in fact, a volume (three dimensions), even though only two of its dimensions are shown on the duplex image. The “thickness” of the sample volume cannot be shown on the two-dimensional spectrum display, and this can sometimes lead to errors of localization. Doppler signals may be obtained from vessels located near the area of interest and marginally within the sample volume but are not shown on the two-dimensional display. For example, the ultrasound image may show the internal carotid artery, but you may actually be receiving flow signals from an adjacent external carotid branch. Second, the actual shape and size of the sample volume may be somewhat different from the linear representation shown on the duplex image. Third, and most important, the Doppler spectrum displays blood flow information obtained within the sample volume and does not provide information about blood flow in other portions of the vessel visible on the ultrasound image. Therefore if the sample volume is positioned incorrectly, key diagnostic information may be overlooked.How to determine the direction of flowThe frequency spectrum shows blood flow relative to the transducer . Flow in one direction, toward the transducer, is displayed above the spectrum baseline, and flow in the opposite direction is shown below the baseline. One must always remember that the flow direction is relative to the transducer and is not absolute. The apparent direction of blood flow can be reversed by turning the transducer around or by pressing a button on the instrument that inverts the spectrum! The arbitrary nature of this arrangement can lead to significant diagnostic error. How often is reversal of flow in the vertebral artery missed? Clues to the correct direction of flow can be found by comparing the color (e.g., red or blue) in the vessel with the color bar or color velocity scale and by checking whether the velocity information on the spectrum is positive (toward the transducer) or negative (away from the transducer). Another method to check direction of flow is comparison with a reference vessel in which the flow direction is known (e.g., when working in the abdomen, the aorta is a handy reference vessel).Wave Analysis PulsatilityIn arteries, each cycle of cardiac activity produces a distinct wave on the Doppler frequency spectrum that begins with systole and terminates at the end of diastole. The term waveform refers to the shape of each of these waves, and this shape, in turn, defines a very important flow property called pulsatility . In general terms, Doppler waveforms have low, moderate, or high pulsatility features, as illustrated in Fig. 3.3 . Please review the three types of pulsatility on this figure before proceeding to the following discussion.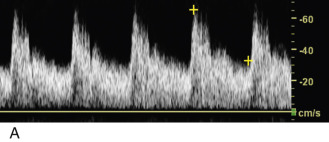 FIG. 3.3 Pulsatility. (A) Low pulsatility is indicated by broad systolic peaks and persistent forward flow throughout diastole (e.g., the internal carotid artery). (B) Moderate pulsatility is indicated by tall, sharp, narrow systolic peaks and relatively little diastolic flow (e.g., the external carotid artery). (C) High pulsatility is characterized by narrow systolic peaks, flow reversal early in diastole, and absence of flow late in diastole. In this classic triphasic example, the first phase ( 1 ) is systole, the second phase ( 2 ) is brief diastolic flow reversal, and the third phase ( 3 ) is diastolic forward flow. Triphasic flow is seen in normal extremity arteries at rest.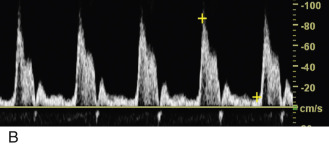 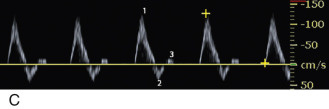 Low-pulsatility Doppler waveforms have broad systolic peaks and forward flow throughout diastole (see Fig. 3.3A ). The carotid, vertebral, renal, and celiac arteries all have low-pulsatility waveforms in normal individuals because these vessels feed circulatory systems with low resistance to flow (low peripheral resistance). Low-pulsatility waveforms are also monophasic , meaning that flow is always forward, and the entire waveform is either above or below the Doppler spectrum baseline (depending on the orientation of the ultrasound transducer). Low-pulsatility waveforms do not demonstrate reversal of flow.Moderate-pulsatility Doppler waveforms have an appearance somewhere between the low- and high-resistance patterns (see Fig. 3.3B ). With moderate flow resistance, the systolic peak is tall and sharp, but forward flow is present throughout diastole (sometimes interrupted by early-diastolic flow reversal). Examples of moderate pulsatility are found in the waveforms obtained from the external carotid artery and the superior mesenteric artery (during fasting).High-pulsatility Doppler waveforms have tall, narrow, sharp systolic peaks and reversed or absent diastolic flow. The classic example of high pulsatility is the triphasic flow pattern seen in an extremity artery of a resting individual (see Fig. 3.3C ). A sharp systolic peak (first phase) is followed by brief flow reversal (second phase) and then by brief forward flow (third phase). High-pulsatility waveforms are a feature of circulatory systems with high resistance to blood flow (high peripheral resistance).https://radiologykey.com/doppler-flow-imaging-and-spectral-analysis/ Low-pulsatility Doppler waveforms have broad systolic peaks and forward flow throughout diastole (see Fig. 3.3A ). The carotid, vertebral, renal, and celiac arteries all have low-pulsatility waveforms in normal individuals because these vessels feed circulatory systems with low resistance to flow (low peripheral resistance). Low-pulsatility waveforms are also monophasic , meaning that flow is always forward, and the entire waveform is either above or below the Doppler spectrum baseline (depending on the orientation of the ultrasound transducer). Low-pulsatility waveforms do not demonstrate reversal of flow.Moderate-pulsatility Doppler waveforms have an appearance somewhere between the low- and high-resistance patterns (see Fig. 3.3B ). With moderate flow resistance, the systolic peak is tall and sharp, but forward flow is present throughout diastole (sometimes interrupted by early-diastolic flow reversal). Examples of moderate pulsatility are found in the waveforms obtained from the external carotid artery and the superior mesenteric artery (during fasting).High-pulsatility Doppler waveforms have tall, narrow, sharp systolic peaks and reversed or absent diastolic flow. The classic example of high pulsatility is the triphasic flow pattern seen in an extremity artery of a resting individual (see Fig. 3.3C ). A sharp systolic peak (first phase) is followed by brief flow reversal (second phase) and then by brief forward flow (third phase). High-pulsatility waveforms are a feature of circulatory systems with high resistance to blood flow (high peripheral resistance).https://radiologykey.com/doppler-flow-imaging-and-spectral-analysis/
| |
|   | | | | Doppler US |  |
|
مواضيع مماثلة |  |
|
| | صلاحيات هذا المنتدى: | لاتستطيع الرد على المواضيع في هذا المنتدى
| |
| |
| |
|


