
موقع د. كمال سيد الدراوي
طبي_ اكاديمي _ ثقافي _ تعليمي _ _ استشارات طبية_فيديو طبي
|
|
| | Doppler US |  |
| | |
| كاتب الموضوع | رسالة |
|---|
د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: dopp Law, mapping, dopp information موضوع: dopp Law, mapping, dopp information  الإثنين مايو 06, 2024 1:00 pm الإثنين مايو 06, 2024 1:00 pm | |
| Color Maps•Doppler shifts yield information regarding velocity•Color Doppler uses a “dictionary” or look-up table to convert•measured velocities into colors.•You can choose the dictionary:•»: velocity mode or variance mode•Velocity Mode : varies up & down•Variance mode : varies up & down•and side-to-side•Color coded Doppler flow mapping (color flow mapping or color Doppler) is a newly developed technology which displays blood flow as color-coded information on the two-dimensional image. This method is an application of the pulsed Doppler method.The speed of the blood flow is shown with a color scale. Usually, blood flow away from the probe is shown in blue, while blood flow toward the probe is red.In color Doppler mode, color assignments are set and displayed as a 'map' on the screen. Traditionally, red is the color assigned to flow towards the transducer, and blue is assigned to flow away from the transducer.Doppler LAWDefinition: Doppler Effect refers to the change in wave frequency during the relative motion between a wave source and its observer. It was discovered by Christian Johann Doppler who described it as the process of increase or decrease of starlight that depends on the relative movement of the star.Creation of a color flow imagehttps://radiologykey.com/creation-of-a-color-flow-image/Ultrasound scanners also use the detected blood velocity, with respect to the ultrasound beam, to form a color map of blood flow superimposed on to the anatomical map provided by pulse echo imaging. This map provides a means for rapid interrogation of a region of interest (ROI) and enables the operator to be selective in the points from which to obtain spectral Doppler information. The development of color flow imaging has greatly extended the capabilities of imaging small vessels and has also allowed for a reduction in investigation time, dramatically increasing the role of vascular ultrasound. The first real-time color flow images were produced in 1985 and were only possible due to the use of different mathematical methods to extract the mean velocity of flow relative to the beam (mean Doppler frequency). This made collection and analysis of the ultrasound echos fast enough to enable the production of color flow maps capable of displaying pulsatile blood flow in real time.COLLECTION OF 2D DOPPLER INFORMATIONThe two-dimensional (2D) color flow map is created by detecting the back-scattered signals from hundreds of sample volumes along each scan line and using over a hundred of scan lines to cover the ROI, as shown in Figure 4.1. The scanner divides the back-scattered signal into hundreds of samples along the scan line, each sample being at a different time delay after the transmitted pulse, and therefore returning from a slightly different depth in the tissue. The depth from which a signal has returned can be calculated from this time delay, using the speed of sound in tissue, in the same way as is used in pulse echo imaging. Several pulses must be transmitted and received along the scan line for the movement of the blood to be detected. Once sufficient samples have been detected from each sample volume to allow estimation of the blood velocity relative to the beam, a second scan line adjacent to the first can be produced. Hundreds of scan lines may be used to produce the 2D color flow image. The estimated mean relative velocity (equivalent to the Doppler frequency) from each sample volume within the tissue can be displayed in color, as shown in Figure 4.2. In this image of an artery lying next to a vein, the Doppler shift frequencies produced by flow toward the transducer are displayed in red, and those produced by flow away from the transducer are shown in blue. The higher relative velocities are shown as yellow and turquoise, whereas the lower relative velocities are displayed as deep red and deep blue.Figure 4.1 The color flow image is created by detecting the back-scattered ultrasound from hundreds of sample volumes along over a hundred different scan lines.In this image of an artery lying next to a vein, the Doppler shift frequencies produced by flow toward the transducer are displayed in red, and those produced by flow away from the transducer are shown in blue. The higher relative velocities are shown as yellow and turquoise, whereas the lower relative velocities are displayed as deep red and deep blueFigure 4.4 The basic elements of a color flow scanner.Figure 4.4 shows the basic elements of a color flow scanner. Before any analysis of the returning echoes is carried out, 1/ the signal is filtered by the clutter filter to remove the high-amplitude signals returning from the surrounding stationary tissue and the slow-moving vessel walls, while 2/ preserving the low-amplitude signals from the blood. 3/ The filtered signal is then analyzed to obtain an estimate of the mean relative velocity (Doppler shift frequency) in each sample volume using the Doppler statistic estimator, as described earlier. 4/ Postprocessing is then used to smooth the data in order to produce a less noisy color image. This can be done by 5/ combining the data obtained from consecutive images, known as frame-averaging. As each point on the image can only be assigned either a specific color or level of gray, a decision has to be made as to whether to display the pulse echo information or any flow information detected. This involves : 6/ the process known as blood–tissue discrimination.https://radiologykey.com/creation-of-a-color-flow-image/NEXT
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:49 pm عدل 2 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Blood–tissue discrimination موضوع: Blood–tissue discrimination  الإثنين مايو 06, 2024 1:28 pm الإثنين مايو 06, 2024 1:28 pm | |
| Blood–tissue discrimination
Generally, the returning pulse echo signals from the vessel lumen are very low in amplitude compared with those from the vessel walls and surrounding tissue. In addition, larger Doppler frequencies are detected from the rapidly moving blood in comparison to the low Doppler frequencies obtained from the slow-moving vessel walls. No Doppler shift would be detected from stationary surrounding tissue. Ultrasound imaging systems are designed with an adjustable control called the ‘color write enable’ or ‘color write priority’ control. This control allows the operator to select the imaging signal intensity above which the gray-scale image is displayed rather than the color information. If a Doppler signal is obtained from an area in which the gray-scale signal is higher than the level set by the operator, the scanner assumes that the Doppler signal results from moving tissue and therefore does not display it. Below this level of gray, providing there is an adequate motion detected, it is assumed that any motion detected originates from blood, and color will overwrite the gray scale in areas where a Doppler signal is detected. If, for instance, the operator wishes to demonstrate flow in a small vessel that does not have an anechoic (echo-free) lumen on the image, the threshold for displaying gray-scale information will need to be increased, thus giving priority to writing color information.Most systems also have a flash filter. This is designed to remove color flashes, known as flash artifacts, that are generated by rapid movement between the transducer and tissue, such as when the sonographer moves the transducer during scanning.Color-coding the Doppler information
Having obtained a value of the mean Doppler frequency present in the multiple sample volumes, these data now have to be displayed on the image. This is done by color-coding the Doppler information. The color on the screen has three attributes : luminosity, hue, and saturation. 1/ Luminosity is the degree of brightness or shade of the displayed color; 2/ hue is the wavelength (i.e., the actual color displayed, from violet through red),3/ and saturation is the degree to which the color is mixed with white light (e.g., from red through light pink, producing up to 20 identifiable tints). These three attributes can be used to produce a variety of color scales, as shown in Figure 4.5, which can be displayed as a bar at the side of the image. The scale usually consists of a different color representing different flow directions, with red often used to show flow toward the transducer and blue depicting flow away from the transducer. Most scanners allow the operator to invert the color scale in order to display flow toward the transducer as blue and flow away as red. This is indicated by inverting the color scale displayed at the side of the image (Fig. 4.5E). It is essential for the operator to be aware of which colors represent which directions of flow within the image, otherwise serious diagnostic errors can occur. Ultrasound scanners provide a range of color scales, and certain scales are more appropriate in particular imaging situations. The various color scales may be selected to accentuate the different parts of the range of detected relative velocities seen in different clinical situations. For example, in an arterial scan, the color scale may accentuate the differences in the upper portion to highlight velocity changes in the higher range of velocities.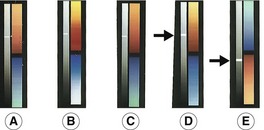 https://radiologykey.com/creation-of-a-color-flow-image/ https://radiologykey.com/creation-of-a-color-flow-image/
عدل سابقا من قبل د.كمال سيد في الجمعة مايو 31, 2024 6:17 pm عدل 2 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Aliasing phenomenon (ultrasound) موضوع: Aliasing phenomenon (ultrasound)  الجمعة مايو 10, 2024 12:22 pm الجمعة مايو 10, 2024 12:22 pm | |
| Aliasing phenomenon (ultrasound)Aliasing is a phenomenon inherent to Doppler modalities which utilize intermittent sampling in which an insufficient sampling rate results in an inability to record direction and velocity accurately Physics
Unlike continuous wave Doppler (CWD), pulsed wave (PWD) and color flow Doppler (CFD) modalities [alternate between rapid emission of ultrasound waves (at a rate termed the pulse repetition frequency ]PRF]) and reception of incident ultrasound waves]. The time an ultrasound wave travels, given a constant speed in soft tissue (c = 1540 meters/second) will correspond to the distance traveled. Pulsed wave Doppler and color flow Doppler operate on this presumption; when a location of interest is designated, the ultrasound machine will only record returning echoes during an interval that corresponds to the time necessary for wave egress and return [Go Return Time] along a linear path. If [Doppler shifts # occur at a frequency exceeding the maximum pulse interval (1/pulse repetition frequency) detected phase shifts will be calculated based on incorrect assumptions] The Nyquist limit defines the frequency at which aliasing and range ambiguity will occur, and is equal to thePRF/2.
Factors such as @ higher velocities of target structures and @ increasing depth of the region of interest insonated will result in aliasing and consequent range ambiguity {Pulsed Doppler ultrasound (PW) can be used to determine the location of frequency shifts within the cardiac chambers or great vessels. However, it is possible to record similar frequency shifts at sample volume locations distal to their original site; this is referred to as range ambiguity (RA).}. Other potential causative factors include
- use of higher frequency transducers
- inappropriate angle of insonation
- ,large sampling volume
Clinical use
EchocardiographyA specific use for aliasing in echocardiography is 1/ the calculation of the {EROA} effective regurgitation orifice area in the assessment of valvular regurgitation, most commonly involving the mitral valve. With color Doppler interrogation of a mitral regurgitant jet, a hemispheric flow convergence forms surface area tapering to form the vena contracta before entering the left atrium. The hemispheric area, Proximal Isovelocity Surface Area (PISA) is calculated and the product of PISA and aliasing velocity yields regurgitant flow. The quotient with calculated MR regurgitant VTI yields EROA ..{The Velocity Time Integral (VTI) is a clinical Doppler ultrasound measurement of blood flow, measured by the area under the wave curve and equivalent to the distance traveled by the blood}. .Pulsed wave DopplerIn case of spectral Doppler the velocity peak is cut off at the peak of the scale, and the peak is displayed at the bottom of the scale, often overlapping with the rest of the curve. The artifact {Aliasing} can be quickly remedied by 1/ lowering the baseline (if display of flow away from the transducer is not required), or 2/ increasing the PRF.Color flow DopplerIn color Doppler aliasing 1/ is encountered as red to blue hues immediately adjacent to each other in a vessel, which is - unlike in case of true flow reversal - not separated by a black region of no flow.2/ The artifact immediately disappears if the upper margin of the velocity scale is increased above the peak flow velocity. Color aliasing 3/ is useful for detecting foci of increased flow (e.g. stenosis, arteriovenous fistula).4/ Note that aliasing does not occur with power Doppler, as it does not display velocity 2.Aliasing occurs in color Doppler 5/ when the speed of blood flow exceeds 0.4-0.7m/s 6.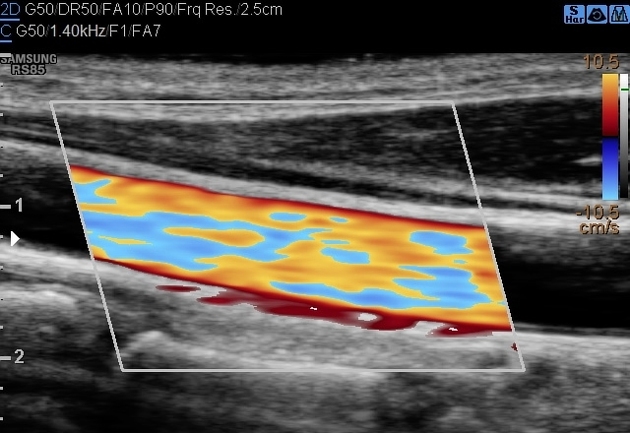 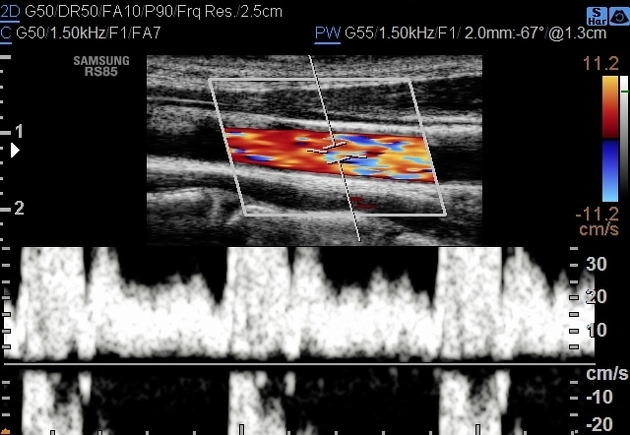 Quiz questions
https://radiopaedia.org/articles/aliasing-phenomenon-ultrasound?lang=us
عدل سابقا من قبل د.كمال سيد في الجمعة مايو 31, 2024 6:18 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Color Comet Tail/Twinkling Artifact موضوع: Color Comet Tail/Twinkling Artifact  الجمعة مايو 10, 2024 5:29 pm الجمعة مايو 10, 2024 5:29 pm | |
|
عدل سابقا من قبل د.كمال سيد في الجمعة مايو 31, 2024 6:20 pm عدل 2 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: 3D/4D image acquisition موضوع: 3D/4D image acquisition  الجمعة مايو 17, 2024 7:35 pm الجمعة مايو 17, 2024 7:35 pm | |
| How to acquire a nice 3D/4D image 1st yu have to obtain a good 2D image : Press power buttonPress select probeSelect OB ist or 2nd trim scanInsure probe marker & orientation correctlyStatic 3D: means one single volume 3D image. Only a set of 3D volumetric data is captured.4D: means to acquire real time 3D images multiple sets of 3D volumetric data within a continuous time frame is acquired & allined chronologically..The best plane to get a good 3D/4D image, is the middle sagittal planeIst yu should obtain the BPD imaging planeThen rotate probe 90 to obtain the sagittal plane.If yu are not in the sta dard mid sagittal plane, just adjust probe slowly to get the middle sagittal plane. When yu get the midsagittal plane, the 2D image preparation work is ready.Step 23D scanningPress the 3D button on the control panel.Then the ROI will show up.use the set key & trackball to adjust the size of the ROI & move it to the appropriate position.The size of (ROI) Reion of interest should be appropriate, not too small, not too large.Moove the ROI to contain the whole fetal head, without any blockage.Improper volume (VOL) can't get good & complete 3D image.Use the (set) key to activate the VOL curve & adjust it with the trackball moving aa close to the fetal face surface as possible.Press (uldate) key on the control panel to start the 3D image acquisition.The acquisition process is being done automatically.During the period, please maintain the probe in the still position.Step 3 (4D scaninng)Press the (4D) key on the control panel, then the ROI will show out.Use the (set) key & trackball to adjust the size of the ROI & moove it tl the appropriate position.Press (update) key on the control panel to enter the 4D image real-time display status.Press the (freeze) key on the control panel to freez the image..The the 4D image will automatically be terminated. https://www.facebook.com/search/top/?q=ultrasound%20step%20by%20step
عدل سابقا من قبل د.كمال سيد في الجمعة مايو 31, 2024 6:24 pm عدل 2 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: doppler US Basics موضوع: doppler US Basics  الإثنين مايو 20, 2024 5:19 pm الإثنين مايو 20, 2024 5:19 pm | |
|
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:42 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Revision dopp equation,PWD موضوع: Revision dopp equation,PWD  الجمعة مايو 24, 2024 12:05 pm الجمعة مايو 24, 2024 12:05 pm | |
| •What is the principle of ultrasound?
An electric current passes through a cable to the transducer and is applied to the crystals, causing them to deform and vibrate. This vibration produces the ultrasound beam. The frequency of the ultrasound waves produced is predetermined by the crystals in the transducer.
•There are two successive Doppler shifts involved:
•First, the sound from the stationary transmitting TXR is received by the moving erythrocytes.
•Second, the erythrocytes act as moving sources as they
•re-eradiate the US back toward the transducer, which is now the stationary receiver.
•These two Doppler shifts account for factor 2 in the
•Doppler equation:
Doppler Equation :
•fd = ft – fr = 2 ft v cos^(ceta) / C
•where: fD is the Doppler shift, ft is the transmitted frequency, fr is the received frequency, v is the blood velocity, θ (ceta) is the insonation angle (the angle between the US beam and the blood flow), and c is the speed of sound.
•The Doppler shift is thus directly proportional to the velocity of the flow, (v), to cosine of the insonation angle, θ, and to the transmitted frequency of the US, ( ft).6
•What is the principle of ultrasound?
An electric current passes through a cable to the transducer and is applied to the crystals, causing them to deform and vibrate. This vibration produces the ultrasound beam. The frequency of the ultrasound waves produced is predetermined by the crystals in the transducer.
Angle of insonation is defined as the angle of the ultrasound beam relative to the tissue or organ of interest. The strongest echoes are produced when the angles of incidence approach the angle of reflection.
SEE fig next slide
The Greek letter θ (theta) is used in math as a variable to represent a measured angle. For example, the symbol theta appears in the three main trigonometric functions: sine, cosine, and tangent as the input variable.
Pulsed doppler
The Doppler circuitry determines the change in frequency indirectly. With a series of pulses the phase of the returning signals are compared with the phase of the emitted signal.
A change in phase translates to a change in frequency; eg, when the returning signal is compared with the emitted one, wave tops will not meet wave tops because the distance between wave tops has changed. The number of these pulses per second is called the pulse repetition frequency (PRF).
Insonation angle, (Doppler angle)
This is the angle between the path (TXR) of the Doppler pulses and the direction of flow in the vessel.
When this angle is 90°, there will be no frequency shift as can be seen from the equation above: cos(90°) = 0.
The maximum frequency shift of a given vessel is obtained when the direction of flow matches the direction of the Doppler pulses (Doppler angle = 0, flow directly towards or away from the transducer).
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:41 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Revision blood velocity, dopp shift موضوع: Revision blood velocity, dopp shift  الجمعة مايو 24, 2024 12:44 pm الجمعة مايو 24, 2024 12:44 pm | |
| Blood velocity versus Doppler shift
The Doppler circuitry determines the change in frequency and, this may only be translated into a blood velocity if the insonation angle is recorded and is included in the calculation. Nevertheless, all newer equipment report blood velocities (both in spectral Doppler and on the colour bar) assuming that the Doppler angle is zero. This is, however, more often wrong than right and we are in fact dealing with frequency information unless angle correction has been performed (the process of informing the machine of the insonation angle).
Angle correction is only possible in spectral Doppler and is not an issue in a rheumatological setting.
COLOUR DOPPLER, VELOCITY DOPPLER AND COLOUR FLOW MAPPING
In CFD, real-time presentation of flow information in colour is superimposed on the grey-scale morphological image.
In colour Doppler, analysis is performed in the colour box, which is divided into cells.
Each cell behaves like an independent Doppler gate with its own Doppler analysis.
The mean frequency shift for each cell is computed and displayed as a colour.
The colours that arise from the detected Doppler shifts primarily indicate qualitative direction of flow.
Generally, red is used to indicate a flow towards the transducer and blue away from the transducer.
Different hues of red (or blue) indicate different velocities (in reality different frequency shifts).
Lighter hues are used to indicate higher frequency shifts. Interpreting the colours
The Doppler circuitry merely detects movements up and down in the image plane.
A dark red spot may therefore be blood moving slowly, directly towards the transducer or blood moving quickly at an angle close to 90°.
As we generally do not know the insonation angle to the vessels we cannot compare velocities between vessels.
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:38 pm عدل 2 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Revision PD & dopp Paramters موضوع: Revision PD & dopp Paramters  الجمعة مايو 24, 2024 12:52 pm الجمعة مايو 24, 2024 12:52 pm | |
| POWER DOPPLER (ENERGY DOPPLER)
PD displays power of the Doppler shift in each cell instead of the mean frequency shift. This gives PD a theoretical advantage over colour Doppler with regard to sensitivity. Disregarding direction of flow (negative or positive frequency shift) and disregarding velocity (high or low frequency shift) the power (energy) of the many different frequency shifts inside a cell are added to form the power signal.
The power mode does not measure velocity or direction and is very sensitive to flow. Therefore, it is almost angle independent and without aliasing.7
The wall filter in ultrasound is a way of filtering out low or high frequency Doppler signals. ...
In clinical ultrasound, it is usually used to filter out very low frequencies that may add noise to a spectral Doppler waveform.
A typical use is removing the low frequency reverberation of an arterial wall.
� DOPPLER PARAMETERS
The most important adjustable parameters are Doppler frequency, Doppler gain, PRF, colour priority, filter, focus, persistence, colour box position and size.
Patient positioning and scanning technique further influence the quality of the Doppler examination.
Doppler frequency
A lower Doppler frequency will allow more penetration but also a more grainy Doppler image (larger colour pixels). Thus, higher Doppler frequency gives a more detailed image of the vessels but at the expense of penetration.
The trade-off between penetration and sensitivity is somewhat unpredictable and resolution is in this context really not an issue.
The ability to depict slow flow in a small vessel (with a weak Doppler reflection) is enhanced by a lower frequency (because the weak reflection has more penetration) but is also enhanced by a higher frequency because the Doppler shift is higher (if the reflection is powerful enough to penetrate).
The optimum frequency must be found in practice and not in theory.
Colour box
The numerous Doppler analyses inside the colour box are quite demanding on computing power of the US unit.
The frame rate goes down when colour is added and in order to obtain as live an image as possible (high frame rate) it is therefore generally recommended to make the box as small as possible.
We do, however, recommend always letting the box go to the top of the image in order to be aware of reverberation artefacts (see reverberations).
Scale and pulse repetition frequency
PRF is the Doppler sampling frequency of the transducer and is reported in Hz.
The maximum Doppler shift frequency that can be sampled without aliasing is PRF/2, which is called the Nyquist limit.8
The Nyquist limit may be presented on-screen as a blood velocity (the maximum measurable velocity of blood moving directly towards or away from the transducer) or in Hz (maximum measurable Doppler shift).
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:37 pm عدل 2 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Revision filters, gain, persistence موضوع: Revision filters, gain, persistence  الجمعة مايو 24, 2024 12:59 pm الجمعة مايو 24, 2024 12:59 pm | |
| If the blood velocity is above the Nyquist limit, the machine will misinterpret the velocity and aliasing will occur. This is not an issue with PD.
The sensitivity of both colour Doppler and PD is affected by PRF adjustments. When a high PRF is chosen it is assumed that the investigator is interested in high velocities, and therefore filters that remove low flow to remove noise are applied (so-called linked controls).
Selecting a high PRF therefore makes the system insensitive to lower velocities because of the linked controls.
Colour priority (threshold)
When colour information is obtained, grey-scale information will often also be present and the machine has to decide whether to show one or the other.
Colour priority is a function that makes this decision for the machine. This function allows valid grey-scale information to override false Doppler information, eg, it helps suppress motion artefacts in the relatively hyperechoic tissue surrounding a pulsating artery (above a certain grey level, grey overrides colour).
This function also allows supposedly valid Doppler information to override false grey-scale information, eg, inside vessels colour overrides the relatively weak grey-scale reverberation artefacts (below a certain grey level colour overrides grey). This function explains why some Doppler artefacts apparently prefer to appear in dark regions of the image. It also explains why grey-scale gain may influence the amount of colour in the image (increasing grey-scale gain may result in more grey information being above the threshold where colour is suppressed).
Filters
Every Doppler instrument has high-pass filters, which eliminate the lowest Doppler shifts from the display.
The Doppler shifts originate from motion of the vessel wall and solid tissue.
These unwanted shifts are referred to as clutter or motion artefacts.
The filters—also called wall filters—may, however, eliminate signals from low velocity flow as the filters separate by frequency alone.9 10
The PRF and wall filter are linked controls—the lowest possible wall filter is lower for a low PRF than a high.
The filters should be kept at their lowest setting for use in rheumatology.
Gain
The Doppler gain is independent of grey-scale gain.
The gain setting determines the sensitivity of the system to flow.
By lowering the gain, noise and motion artefacts may be prevented but weak flow signals will go undetected.
11 A gain setting that is too high results in random noise.12
It is appropriate to set the Doppler gain by turning it up until random noise is encountered and then lowering it until the noise disappears.11
Persistence
Persistence is a function that averages colour information over a number of frames.
Most brochure images are made with maximum persistence because this results in all colour information over time being displayed in one image.
All vessels are then filled with colour. The dynamic nature of flow is, however, lost.
With low or no persistence the high or low resistance nature of arterial flow may be seen as blinking colour foci or colour foci with pulsating intensity, respectively.
In a rheumatological setting there is no advantage with high persistence
Patient positioning
The patient must be positioned comfortably, and the area under investigation must be completely relaxed; otherwise, tension in the muscles and tendons will produce slight tremor resulting in movement artefacts. When scanning the hand and elbow regions, the arm should not rest on the abdomen or thorax because of respiratory movement. Some patients should also keep quiet during the Doppler examination because the voice itself may produce movement artefacts and because some patients cannot talk without involuntary movement of the hands.
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:34 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Revision scanning technique موضوع: Revision scanning technique  الجمعة مايو 24, 2024 1:19 pm الجمعة مايو 24, 2024 1:19 pm | |
| Scanning techniqueMost important in Doppler examinations is that very little pressure should be applied by the transducer. The pressure will affect the haemodynamics with resulting decreased flow. The use of generous amounts of scanning gel with visible gel between the transducer and skin will ensure light pressure.FocusingThe Doppler uses the same focus point as the grey-scale image. In the focal zone, the pulse is most narrow and the pulse therefore has higher spatial peak energy. As a consequence, the echoes generated in the focal zone have higher amplitudes. It is therefore not surprising that the Doppler is very dependent upon focus positioning . Some machines help us to some extent. When Doppler is activated, these machines move the focus point into the colour box (if it was outside) and then to a predetermined position inside the box. If multiple focus points were in use, the machine changes that to single focus point and then inside the colour box. Still, within the colour box focus positioning affects flow detection. Substantial differences may be falsely generated or falsely overlooked in longitudinal studies if the focal point is not consistently in the area under investigation.PressureFalse findings of absence of flow may occur if the examiner presses too hard on the tissue with the transducer, thereby blocking the flow. When scanning a concave or convex surface it may be tempting to press the surface flat with the transducer. Instead, a generous amount of scanning gel should be used, which obviates the need for pressure to obtain good acoustic contact. Color MapsDoppler shifts yield information regarding velocityColor Doppler uses a “dictionary” or look-up table to convertmeasured velocities into colors.You can choose the dictionary:» velocity mode or variance modeVelocity Mode : varies up & downVariance mode : varies up & downand side-to-side 
عدل سابقا من قبل د.كمال سيد في الجمعة مايو 31, 2024 6:25 pm عدل 2 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: doppler frequency,wavelength, velocity موضوع: doppler frequency,wavelength, velocity  الجمعة مايو 24, 2024 1:35 pm الجمعة مايو 24, 2024 1:35 pm | |
| •The sound is a mechanical power (energy) which travel or propagate during flexible (elastic) continuous medium by the rarefaction and compression of elements that compose it. Rarefaction is an area where the elements furthest from each other, whereas the compression is an area where the elements are closest together.
* The energy (power) traveling occurs when the signal wave front in the direction of power propagate, called as a longitudinal wave. The distance between both of rarefaction and compression or between each two spots which regenerate on the sinusoidal signal wave known as the wavelength (λ).
•In contrast, the quantity of times the signal wave fluctuates (oscillates) during a cycle count each second known as the frequency (f).
* Frequency is the number of vibration cycles that occur
•in 1 sec.
* When the frequency exceeds 20KHz, the human cannot hear it, and this process called ultrasound.
•The speed of sound relies on both the compressibility and density of the medium and variates largely with materials variation.
* The relationship between the wavelength (λ), frequency, (f), and the velocity (c) given by this formula :
* (f)/(c)=(λ)
•The US beam travels like a longitudinal signal wave from the probe surface area into the medium, and displays two beam models: a diverging beam (far field) and a converging beam (near field).
•However, both the frequency of emitted sound and probe diameter determine the near-field length in unfocused single element probe.
•The Doppler effect of sound is sometimes the common case in our lives.
•For instance, consider understanding and realizing the influence of the sound on the hearing, like a vehicle approaching and then go away from a listener. The pitch of sound increases when the car approaches then suddenly sound pitch decrease as the car moves away from the listener.
•The rising frequency or pitch of the sound waves displays the constant frequencies from the ear and to the known rise in frequencies from the velocity of the vehicle in motion toward the listener. When both the vehicle and listener are constant, the wave pulse frequency of the vehicle at eardrums is stationary.
•This principle of car and listener is identical to the principle of B-mode in an ultrasound system.
•In B-mode, both the source (probe) of the ultrasound pulse frequency and target tissue are nearly constant.
•Thus, the frequency pitch of the transmitting ultrasound pulse waves and also the frequency pitch of the returning signals echoes are identical.
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:31 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: doppler equation موضوع: doppler equation  السبت مايو 25, 2024 7:17 am السبت مايو 25, 2024 7:17 am | |
| •No proportional motion from pulse to pulse when the flow is vertical (perpendicular) on the beam.
•Thus, the Doppler signal size is based on many factors :
•1- The first one is, blood speed : as speed increases, the Doppler frequency also increases.
•2- Second, US frequency: rising ultrasound frequency will produce high Doppler frequency.
•Like in B-mode, when the ultrasound frequencies decrease, the penetration will improve.
•3- Finally, the angle of insonation: when the beam of ultrasound has much aligned toward the direction of the flow, the Doppler frequency will rise (the angle of insonation between the medical ultrasound beam and the blood flow direction becomes smaller).
•Doppler ultrasound supply is an instrument, which it is using for measuring the blood speed and flow, also it is utilized in the research field and clinical field investigations to quantify the range and influence of arterial disease.
•In Doppler imaging of the blood, the constant object usually is the probe, and the shifting reflectors that produce the returning signal echoes are originally the red cells.
•The Doppler shift frequency or the Doppler-shift is known as the variation between the frequencies of transmitted and received of ultrasound waves echoes.
•Doppler equation :
•ΔFT = (2fo v cosθ/c)
•the Cos theta or cos θ is the ratio of the adjacent side to the hypotenuse, where θ is one of the acute angles.
•The cosine formula is as follows:
•Cos \Theta = \frac{Adjacent}{Hypotenuse}
The Cos theta or cos θ is the ratio of the adjacent side to the hypotenuse, where θ is one of the acute angles. The cosine formula is as follows: Cos \Theta = \frac{Adjacent}{Hypotenuse}
• How do you calculate cosine of an angle?
•In any right angled triangle, for any angle:
•The sine of the angle = the length of the opposite side. the length of the hypotenuse.
•The cosine of the angle = the length of the adjacent side. the length of the hypotenuse.
•The tangent of the angle = the length of the opposite side. the length of the adjacent side.
•For example, moving of red blood cells at a velocity of :
•1 m/sec toward the vibration pulses transmitted by an US probe & cos seta 1.5
•5 MHz is the US pulse frequency of the probe, 5 MHz is equal to 5 × 106 Hz.
•Doppler equation : ΔFT = (2fo v cosθ/c)
•By applying the Doppler shift formula above :
•5000000/1540=4.214
•6490/4.2= 1.5
• The Doppler-shift is positive and is approximately 6490 Hz.
•ΔFT=(2fo v cosθ/c)
•Where,
•ΔFT : Shift Frequency or Doppler Frequency;
•fo: Ultrasound probe Frequency (Hz);
•V: The blood velocity;
•Cosθ: Cosine Angle of the Insonation;
•C: Speed Sound in Soft Tissue which is equal to1540 m/s.
•When the velocity of sound of source (blood) is zero and the frequency of observer (probe or transducer) is constant, there is no Doppler shift in this case, or it is equal to zero and the wave pulse will be concentric in the center Vsource(blood)= 0. However, when the wave pulses transmitted through the motion between the blood and the probe, the wave pulse will be front of concentric and stay no longer, and the Doppler shift increase when the blood move approaches the transducer, and decrease when moving away from the transducer.
• Vsource (blood)< Vsound.
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:29 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: doppler modes موضوع: doppler modes  السبت مايو 25, 2024 9:26 am السبت مايو 25, 2024 9:26 am | |
| When the velocity of blood and probe are identical, the peak of transmitted signal wave reaches the probe with blood together (Vsource(blood)= Vsound.)
Finally, the transmitted signal wave arrive to the probe after passing the blood at supersonic speed
There are three essential levels of Doppler US that can be carried out, with any level adding data to the previous level.
(1) The initial level is the conventional scale mode OR B-mode gray-scale scanning, in this level, NO Doppler effect is used.
(2)The second level adjusts a color Doppler examination in the region of interest (ROI).
This level produces an image that displays the blood flow in the vessels.
(3) The final level adjusts a small examination area, named a sample volume or gate, along with a vessel of interest.
�Normal protocols contain common carotid artery (CCA) and Doppler ultrasound examination with a good-resolution linear array probe (5–15 MHz).
Three manners should be utilized :
(1) B-mode gray scale imaging,
(2) color Doppler flow (CFD),
(3) and duplex imaging.
B-mode ultrasound imaging of blood flow (1)
A gray-scale of an ultrasound image with two dimensions is called B-mode ultrasound image, and representing the boundaries of both organ and tissue in a slice over the body. B-mode represents the brightness-mode because all pixels in the image are strength power adjusted, that means the brightness-mode of each pixel is relative to the power strength of the ultrasound reflected from the identical structure within the organ body.
In the field of medical ultrasound, B-mode imaging is emitting into the body in a group of short pulses usually 0.2 μs through duration period.
However, to specify the diameter of a sample in B-mode ultrasound image, using the calipers which appear on the control panel of the ultrasound device.
The depth of a reflecting sample can be studied by calculating the time trip between the sending of the ultrasound pulse and the receiving of the reflected signal wave.
Color Doppler imaging of blood (CDI) (CFD) (2)
There are two ways for color ultrasonic imaging estimation: A/pulse wave (spectral Doppler) and B/ color-flow modes. The spectral mode testing the blood speeds of particular arteries. Whereas, color-flow mode utilize color-Doppler signals overlie on a B-mode scan image of the artery to evaluate its vascularity. Both ways depend on the Doppler-shift frequencies.
@ Thus, when the signal wave of blood cells (source) is constant or moving in a parallel direction to the probe, there is no variation between transmitted and receiving frequencies, and in this case, the color Doppler signals undiscovered.
@ The positive Doppler frequency occurs when the source flow approaches toward the probe and the receiving signal frequency wave is higher than the emitting frequency.
@ While, a negative Doppler signal frequency occurs when the blood cells move away from the probe, or, in other words, when the frequency of the emitting signal is higher than returning frequency.
The sample length pointer consists of parallel lines on both parts of the sample or arterial axis line.
The sample length should be positioned within an arterial lumen, and the scale of the sample length size is typically between 0.33 and 0.5 mm of the luminal diameter.
This process effectively produces the Doppler signal back scatter from the sample length which should be low and <2.5 mm.
Then, the Doppler signal is cross over a wall filter which is should be low, and its main function is to reject any noise in the signal caused by low frequency identical to constant or very slow-moving tissue, inclusive a part of the vessel wall(s) The filtered products are then come into a spectrum.
As mentioned above, that there are two ways for color ultrasonic imaging estimation :.
First, in spectral Doppler mode,
First, in spectral Doppler mode, the spectral sends beams pulsed US into the blood flow with a particular PRF.
The PRF is usually between 64 and 128 A-lines, it resulted from sending and receiving ultrasound beams pulses in a particular direction.
To measure the speed of blood flow at a particular depth, the A-lines represent the time-gated to take signals from a wanted depth
The diversities of blood flow speed are displayed as a graphical signal wave shape or image resulted by moving blood called spectrum.
The spectrum appears on the spectrum window which represents the mix of Doppler frequencies existing in a particular sample of a vessel during a short period and displaying the normal flow of blood at a regular velocity.
When the arteries are normal, the flow acceleration in systole is fast, thus, the peak speed arrives within a few hundredths of a second after the contraction stage of ventricular chamber begins.
Furthermore, blood in the middle of the artery shifts quicker than blood at the peripheral side (due to vessle wall resistance), which is known as laminar flow.
The erythrocytes move at an identical speed when the flow is laminar.
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:28 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Doppler parameters موضوع: Doppler parameters  السبت مايو 25, 2024 9:54 am السبت مايو 25, 2024 9:54 am | |
| This spectrum supplies three functions :
1- Time-average maximum velocities (TAMV or mean velocity [Vm]),
2- maximum velocities values as peak systolic velocity (PSV or Vp),
3- and end-diastolic velocity (EDV or Vd).
Initially, the PSV is the highest spot along the length region of the spectrum, whereas EDV is the finish spot of the cardiac cycle. TAMV is the highest average speed values.
Pulsatile (pulsatility) index (PI) and resistance index (RI) are calculated using the proportion of the three velocities measurements (TAMV, PSV, and EDV).
To make an accurate spectral graphic in real human and animal, it is critical to put the sample gate (sample length) Doppler into an artery.
Ordinarily, this may be difficult considering the vessels diameters and the human or animal mobility.
Pulsatile (pulsatility) index (PI) and resistance index (RI) are calculated using the proportion of the three velocities measurements (TAMV, PSV, and EDV).
To make an accurate spectral graphic in real human and animal, it is critical to put the sample gate (sample length) Doppler into an artery.
Ordinarily, this may be difficult considering the vessels diameters and the human or animal mobility.
Adjustment of the Doppler angle is required to measure blood speeds.
Doppler angle is the angle of crossing of the US signal pulse with the direction of moving blood cells.
To make a precise spectrum a Doppler angle of the range between 30° and 60° is required because the function of cos angle has curve above these angles and there is risk of errors and low accuracy in angle correction.
When the Doppler angle is 0°, the top Doppler shift will be done since the cosine of 0° is 1.
When the Doppler angle is 0°, the top Doppler shift will be done since the cosine of 0° is 1.
On the other hand, when the Doppler angle is 90°,
NO Doppler shift (no flow) will be listed, since the cosine of 90° is 0.
It has been displayed that the peak systolic speed values can change with the Doppler angle applied.
Generally, smaller angles will produce lower speeds
PI = (PSV/EDV)/TAMV
RI = (PSV/EDV)/PSV
Uterine artery spectral doppler : PSV 21.3/ EDV 6.5 /TAMV 10.3/� PI (PSV-EDV/MV) =1.442�RI (PSV-EDV/PSV) = 0.695 Second way for color ultrasonic imaging estimation : go back to (slide 25) is color-flow mode, which provides a direct qualitative estimation of the blood flow to various tissues and organs.
The vascularity of the sample is evaluated subjectively taking into account the extension of the sample (artery) with color pixels through a continuous real-time test.
Compared with the spectral mode, color-flow mode is faster, simpler, and more effective way for evaluation than the spectral mode.
The modern Doppler devices show two various modes of color-flow scanning: color-flow and power-flow modes.
The modern Doppler devices show two various modes of color-flow scanning : color-flow and power-flow modes.
The conventional color-flow mode utilizes two special colors (Red and Blue).
Generally, the difference between red and blue colors, used to appear the vascular blood perfusion of the sample (artery). Furthermore, indicate the direction of the blood relation to the probe.
By convection way, red color specks represent blood flow moving toward to the probe, whereas blue color specks indicate red blood cells moving away from the transducer.
However, in power-Doppler flow mode, the motion of blood flow is graduated utilizing a single color, which differs according to the strength of the Doppler signals.
Power-Doppler imaging has : @ major sensitivity to slow (weak) blood flow,
@ and the power-Doppler mode is not related to the Doppler angle.
@ Thus, power Doppler mode can betterment the estimation of vessels with tiny (small) diameters and weak blood flow.
However, color gain indicates the amplification of information flow to improve the photograph of flow.
Color gain (the “gain” knob on the US device) should be highly adjusted without showing background color noise.
The color speed (velocity) is the scale of flow speeds that are depicted in color Doppler US technique.
If the speed scale (the “scale” knob on the US machine) adjusting is lesser than the flow speed of the artery, aliasing artifacts will exist.
The sonographer can reveal the color flow within an arterial lumen by rising the gain or reducing the scale.
In addition, when the gain decreases, the color flow artifacts will decrease.
(3) the 3RD manner of the protocols which should be utilized other than B-mode grey scale & Color doppler: slides(18 & 19)
Duplex imaging
Duplex imaging gathers both the B-mode and pulsed signal wave Doppler (spectral Doppler). The probe is identical to a B-mode imaging probe but with a little group of the probe elements applied to send and discover pulsed Doppler signals.
The residual elements utilize the B-mode imaging.
This mechanism lets the : @ blood vessel to be scanned
@ and the depth of sample is adjusted by an option on-monitor screen cursor called the “Doppler gate.”
The Doppler gate width can be changed to alter the depth range.
A second mark (cursor) on screen monitor is referred to the “angle.”
The Doppler gate with this angle can be aligned with the direction of the vessel to produce a calculation of the insonation angle with the blood flow thus that speed of blood flow can also be calculated through applying the Doppler formula.
Duplex Doppler scanning technique also helps to measure the volume flow which is performed through measuring the lumen diameter on the B-mode image, the highest flow in systole stage, and calculation of the cross-sectional region.
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:27 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Doppler parameters موضوع: Doppler parameters  السبت مايو 25, 2024 2:59 pm السبت مايو 25, 2024 2:59 pm | |
| When the 4 cardiac cycles or gear pump inflow phantom are
completed, the average flow velocity can be calculated by Doppler spectrum.
The device then calculates the volume flow automatically.
However, the expression is generally utilized by the indicating clinicians when ordering a scanning with the spectral Doppler effect, which mechanically would be further precisely termed as a triplex Doppler since it includes all of :
1- gray-scale (B-scan),
2- color Doppler,
3- and spectral Doppler.
The pulsatility index (PI) (also known as the Gosling index)
is a calculated flow parameter in ultrasound, derived from the maximum, minimum, and mean Doppler frequency shifts during a defined cardiac cycle.
Along with the resistive index (RI), it is typically used to assess the resistance in a pulsatile vascular system.
�The pulsatility index (PI) (also known as the Gosling index)
is a calculated flow parameter in ultrasound, derived from the maximum, minimum, and mean Doppler frequency shifts during a defined cardiac cycle.
Along with the resistive index (RI), it is typically used to assess the resistance in a pulsatile vascular system.
�Pulsatility is an intrinsic property of the cardiovascular system, governed by the resistance differential across the arteriolar bed, which allows the potential energy stored in the elastic, proximal arteries to propagate throughout the microcirculation at a mean pressure consistent with adequate perfusion.
When evaluated as a derived flow parameter using pulsed wave Doppler, it is calculated by one of the following equations:
�When evaluated as a derived flow parameter using pulsed wave Doppler, it is calculated by one of the following
PULSATILITY INDEX : PI = (vmax - vmin) / (vmean)
PI = (peak systolic velocity - minimal diastolic velocity) / (mean velocity)
The operator typically recognises and demarcates maximum (vmax) and minimum (vmin) velocities, while the mean velocity (vmean) is calculated by the ultrasound machine.
Clinical use of PI
Because the calculation of these flow parameters is based on the same Doppler spectrum, possible instrument-dependant errors, or an inappropriate angle of insonation by the user, are mitigated somewhat .
Clinical scenarios in which a PI are calculated include:
1- malignant ovarian lesions
2-Transcranial Doppler
3- carotid artery evaluation for stenosis
4- umbilical vein Doppler
5- fetal middle cerebral artery Doppler
6- fetal middle cerebral artery pulsatility index
7- umbilical arterial pulsatility index
The pulsatility index was described in a 1974 paper by Raymond Gosling (1926-2015) 4, a British biophysicist. He is more famously remembered as working under the team led by Rosalind Franklin when x-ray crystallography was used to investigate DNA. From this work James Watson and Francis Crick inferred the structure of DNA for which they shared the Nobel prize 2,3.
Most Significant Common Information That
Obtained by Doppler Ultrasound Technique
1) Pulsed wave Doppler systems imaging
Pulsed wave (PW) Doppler imaging has the ability of @measuring tissue
@ and blood speed from a limited sample volume.
Range of the time should be known from the probe face. Hence, the additional information regarding
@ the position of the blood scattered which is the main feature of pulsed systems over continuous wave systems.
As those PW systems can do this, the pulse of US is transferred in low bursts, like the traditional B-mode imaging, and the system then converts to receive mode.
The distance resulted from switches and converts is the time between the transmitted and received echo with knowing the speed of sound.
The main disadvantage that appear with PW Doppler, that the PW Doppler is an inherent, and is not a product of discretization for digital analysis.
Since only continuous waves (CW) are the goal to Doppler shifts, the pulsed wave (PW) cannot measure frequency shift via Doppler technique.
Hence, PW systems send many of sequential impulses and the alteration of time (or phase) in the received signals is applied to estimate the Doppler frequency.
Usually, 8–32 pulses are emitted; the tradeoff is between precision (more pulses allow more credible estimate allowed by more pulses) and temporal resolution (it takes longer time to emit extra pulses).
عدل سابقا من قبل د.كمال سيد في السبت مايو 25, 2024 3:26 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Doppler parameters موضوع: Doppler parameters  السبت مايو 25, 2024 3:25 pm السبت مايو 25, 2024 3:25 pm | |
| 2) Determination of the speed of blood flow
The mathematic equations for alteration from both the Doppler frequency and the angle of blood flow speed in the tiny sample volume specified by the sample length are considered as a case for debate of the physics principle of medical ultrasound.
The top border of the speed range is adjusted by the sonographer or operator, to reduce artifacts and to improve the signal show.
PSV (peak systolic velosity) or PV (Peak velocity) is the highest spot over the length region of the spectrum, whereas EDV (end diastolic velocity) or EV (End velocity) is the finish spot of the cardiac (heart) cycle.
TAMV (time average maximum velocity) or TV is the highest speed values average of the peak.
These measurement values are calculated from suitable points or spots of the spectrum and offered numerically (as a numbers or digits) on the monitor of most equipment.
The pulsatility can be low when the Doppler wave appear with a wide systolic outline and gradually reduce toward the direction of the end-diastolic profile.
This wave signal refers to that the vessels provide a vascular bottom that have very low resistance .
High-pulsatility or high marginal resistance appears when the Doppler wave signal with sharp (severe) peak systolic outline profile and an inverted or lost diastolic profile.
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Doppler parameters موضوع: Doppler parameters  السبت مايو 25, 2024 4:12 pm السبت مايو 25, 2024 4:12 pm | |
| Moderate-pulsatility Doppler's shape almost occurs between the low- and high-resistance models.
The region under the profile of the greater amounts of the spectral show is refered to the window .The information which appears on the window border is an index of several simultaneous Doppler frequency shifts of the signal and happens when a lot of the width range of the artery is taken for analysis, or the blood flow is confused.
However, if the blood flow in the vessel is influenced by any turbulence, so the Doppler spectral fills in overall the window border and may overtake the fill value in border which is generating from the laminar flow.
Flow trouble or the flow in several directions produces in a vast range of the Doppler frequency shifts.
Doppler indices (peak systolic velocity, end diastolic velocity and time-average maximum velocities) of blood
Blood flow in the vessel is influenced by two main factors,: first one is the resistance given by the wall of vessel and second one is the pressure variation (blood vessel elasticity) between the ends of the vessel.
While the first agent is specified by @ heart function and then, the@ proportional place of the artery vessel in the cardiac circulatory system,
the second factor based on the main @ physiologic state of the artery vessel @ and the desire for the blood.
Thus, any normal artery vessel in the human organs has a special flow model that appear in Doppler spectral waveforms acquired with the medical Doppler ultrasonography (US), and hence, this indicate to both the physiologic and the anatomic need of the vessel.
There are two main equations for calculating the PI and the RI from appeared spectral (See equations 1 and 2).
(λ) = (c) / (f)
ΔFT = (2fo v cosθ/c)
Both the pulsatility index and the resistive index provide input about both the resistance and blood vessel elasticity or blood flow that has no ability to be acquired from measurements value of the velocity alone.
The influences of difference in artery vessel angulation and diameter are not taken into account in the calculation of these indices.
In other words, the PI and the RI calculation method are not affected by the angle of Doppler flow.
The PI and RI can be applied to represent both the elasticity and resistance of downstream blood vessel.
{The blood in a blood vessel travels down stream from the heart to the organs in the arteries and upstream back to the heart in the veins. in the same vessel,}
The best way to calculate the PI is through subtracting the end diastolic velocity EDV from the peak flow velocity PSV, then dividing by the Vm calculated;
while the RI is calculated utilizing the peak systolic velocity
(PSV) as the denominator or divisor.
Measurements of PSV, ESV, and systolic-diastolic S; D or S/D velocity ratio are significant since the peak systolic velocity
(PSV) is the primary Doppler parameter to be abnormal in stenosis.
Umbilical artery (UA) Doppler indices, i.e., pulsatility index (PI), resistance index (RI), and systolic/diastolic ratio (S/D) calculated from blood flow velocities, are used as an important clinical tool for evaluating fetal wellbeing in high-risk pregnancies and to predict outcome of growth restricted fetuses.
The systolic/diastolic (S/D) ratio of flow velocities was measured as an index of peripheral resistance.
In normal pregnancy the umbilical artery (UA) velocity wave S/D ratio declined from 3.9 to 2.1 during the 20th to 40th week while the uterine artery (UA) S/D ratio remained constant between 1.8 to 1.9.
Uterine artery (UA) PI provides a measure of uteroplacental perfusion (and high PI implies impaired placentation with consequent increased risk of developing :
@ preeclampsia,
@ fetal growth restriction,
@ abruption and
@ stillbirth).
The uterine artery PI is considered to be increased if it is above the 90th centile. | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Doppler parameters موضوع: Doppler parameters  السبت مايو 25, 2024 4:38 pm السبت مايو 25, 2024 4:38 pm | |
| In statistics, a percentile is a score below which a given percentage of scores in its frequency distribution fall or a score at or below which a given percentage fall.
For example, the 50th percentile is the score below which 50% or at or below which 50% of the scores in the distribution may be found.
A 95th percentile says that 95% of the time data points are below that value and 5% of the time they are above that value
A percentile (or a centile) is a measure in statistics.
It shows the value below which a given percentage of observations falls. For example, the 20th percentile is the value (or score) below which 20% of the observations may be found.
Main functions of Doppler device parameters
Velocity : (magnitude & direction) : evaluates the mean Doppler scattered speed.
Range gate : Helps reveal blood flow signal wave.
Sample volume OR (sample length) : evaluates the sensitivity of range gate to make sure if it is extreme sensitive at the centre position of the gate.
Maximum velocity precision : the doppler system evaluation of the maximum doppler scatterd speed. In addition to the precision to reveal the degree of arterial narrowing or stenosis.
Lowest detectable speed : evaluation of the lowest speed that is likely to show unambiguously.
Highest detectable speed : evaluation of the highest speed that it is likely to show unambiguously on both the colour Doppler image or on the PW Doppler spectrum.
The highest speed with some diseases or stenosis may reach up to 500-600 cm/s and can show this speed on the spectrum without aliasing.
Spectral broadening : evaluation of the spectral Doppler broadening which is caused by range of angles.
Flow direction : ability to differentiate between flow towards and away from the probe.
Angle correction : This exam supplies he ability to measure the accuracy of the angle correction by the device.
Wall filter : This exam removes intense signals from the vessel wall motion.
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Doppler parameters موضوع: Doppler parameters  الأحد مايو 26, 2024 12:44 pm الأحد مايو 26, 2024 12:44 pm | |
| Pulse repetition frequency in medical Doppler ultrasound
Frequency of ultrasound signal waves may be constant for sole-frequency probes and may be planned by the user for several frequency probes.
The energy of the signal waves transmitted from the probe as well may be planned by the user to change the scanner sensibility in some styles, this control or plan process is called the voltage amplitude, output, or acoustic power different models.
The probe sends ultrasound signal waves in the form of pulses to let the time for receiving of the echo that return before another wave pulse is emitted.
In most equipment, the Doppler PRF is monitored by rising or reducing the field range of speeds to be sampled.
When the significant vessels of study are close to the probe or the blood flow is high, so the setting of high PRF is required.
In contrast, when the significant vessels of study are far away from the probe or the blood flow of vessels is slow, the setting of low PRF is required
The probe sends ultrasound signal waves in the form of pulses to let the time for receiving of the echo that return before another wave pulse is emitted.
In most equipment, the Doppler PRF is monitored by rising or reducing the field range of speeds to be sampled.
When the significant vessels of study are close to the probe or the blood flow is high, so the setting of high PRF is required.
In contrast, when the significant vessels of study are far away from the probe or the blood flow of vessels is slow, the setting of low PRF is required
Phasicity against phase quantification
The Doppler spectral waveform has phasicity, which is made by the cardiac cycle that produces both the velocity and acceleration as a phasic blood flow, then the blood flow of samples shows as a phasic waveform.
However, there are four types of phasicity .
1/ NONphasic waveform, which occurs when there is
@ a constant flow @ or no acceleration @ or velocity,
@ and the pulse waveform is smooth and flat in shape.
2/ Aphasic waveform, which occurs when there is no velocity, no phase, and no flow.
3/ Phasic waveform, which occurs when there is moderate ripple (superficial slopes and a tiny vertical range between inflections).
4/ Finally, “pulsatile” waveform, which occurs when there is clear ripple (steep or decline slopes and a wide or broad vertical range that placed between inflections)
However, conventionally, radiologists have explained phases in word of : @ acceleration @ alterations @ or inflection spots,: relied on the notice that inflection spots (change in pitch or loudness of the voice) produce audible (heard) sounds at medical Doppler ultrasound.
According to this method, the flow manner is qualified as : 1/“monophasic”: when there is @ a low pulsatility waveforms @ and its flow usually in forward direction,
2/“biphasic” when there are @ two sounds heard through each cycle @ or medium pulsatility Doppler waveforms are distinguished by a) both sharp and tall systolic peaks with b)direct forward flow throughout the diastole.
3/ and as “triphasic” when there is three sounds are heard through each cycle or high great pulsatility Doppler waveforms that have narrow, long, and sharp systolic peaks, a short flow reversal (under baseline) and a forward flow phase.
All of pulsatile, phasic and nonphasic flow waveforms all of them have Phasicity
Aliasing
(on spectral Doppler Waveforms/on Color Doppler) :
1/On Spectral Doppler waveforms
# optimize SP dopp parameters :
Increase Velocity Scale/PRF
Increase Wall Filter
Decrease Gain
Adjust Baseline to prevent Wrap
Increase Angle of Insonation/Correction BUT {keep it 60 degrees or lower}
2/ Aliasing on Color Dopple either :
A) Diffuse Aliasing B) Focal Aliasing
A) Diffuse
# Optimize Dolor Doppler parameters :
Increase Velocity Scale/PRF
Increase Wall Filter
Decrease Gain
Adjust Baseline to prevent Wrap
Increase Angle of Insonation/Correction BUT {keep it 60 degrees or lower}
Aliasing on Color Doppler {Focal aliasing}
# interrogate Vessel with spectral Doppler for elevated PSVs :
@ IF normal, then optimize Doppler Parameters AS for Diffuse Aliasing.
@ IF elevated PSVs, then check for secondary signs of stenosis :
& IF YES, Aliasing is likely to be due to stenosis.
& if NO, Aliasing is likely due to Tortuosity OR AVF | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Basic Doppler US principles موضوع: Basic Doppler US principles  الأربعاء مايو 29, 2024 12:56 pm الأربعاء مايو 29, 2024 12:56 pm | |
| •Doppler ultrasound is a noninvasive test that can be used to measure the blood flow through your blood vessels. It works by bouncing high-frequency sound waves off red blood cells that are circulating in the bloodstream. A regular ultrasound uses sound waves to produce images, but can't show blood flow.
•Doppler ultrasonography is medical ultrasonography that employs the Doppler effect to perform imaging of the movement of tissues and body fluids, and their relative velocity to the probe. Wikipedia
•The Doppler effect (also Doppler shift) is the change in the frequency of a wave in relation to an observer who is moving relative to the source of the wave.
Ultrasound doppler imaging is the ability to estimate and measure blood flow through various veins, arteries and vessels. Generally portrayed as a moving picture on an ultrasound system screen, one can usually recognize a doppler test from the color flow that is visible on the ultrasound image. The color in the image can be interpreted based on measuring blood movement in the specific area being photographed.
Doppler imaging is different than conventional ultrasound imaging in one fundamental way: It doesn’t actually image any structures. Conventional ultrasounds provide images for various structures, organs and veins to diagnose growths, breaks, structural problems, and many other potential ailments. Doppler imaging, on the other hand, projects images simply of blood flow
Due to the non-invasive and non- radioactive nature of the ultrasound doppler imaging, it is a methodology that is globally established and revered (respected). Instead of utilizing radiation or invasive features, the doppler functions the same way as other ultrasound imaging equipment does; employing high pitched sound waves that reflect and are translated into colors, images and various movements.
Doppler imaging is different than conventional ultrasound imaging in one fundamental way: It doesn’t actually image any structures. Conventional ultrasounds provide images for various structures, organs and veins to diagnose growths, breaks, structural problems, and many other potential ailments.
Doppler imaging, on the other hand, is applied to detect blood flow and various potential hazards that can occur within the veins, arteries and vessels.
Doppler imaging is generally used to detect blood clots, identify poorly functioning valves in veins, determine whether an artery is blocked, or recognize decreased blood circulation throughout the body. All of these potential threats to one’s health and life can be observed and prevented through use of doppler imaging
There are different applications that people employ doppler imaging for: cardiac doppler, for example, and examining the blood flow to and from the heart is popular and extremely crucial part of cardiological examinations.
Other popular doppler applications include transcranial doppler (which tracks blood flow through the brain and the head), vascular, and general veins and arterial doppler
Color doppler has two colors, red and blue. Using these colors, it became easier to perform exams and diagnose ailments accurately. Some older ultrasound systems, however, don’t have color doppler, and rely on a black and white screen to diagnose patients.
Nowadays, thankfully, nearly all ultrasound machines uses color doppler
Colors on the screen represent blood flow that is in motion.
Blood moving towards the transducer (TXR) is red, and blood moving away is blue. The lighter the shade of red or blue, the more rapid and quick the blood flow. The darker the shade, the slower the blood is moving.
Power doppler, a newer and more advanced form of doppler imaging, is used to provide doppler images for areas that are more difficult, for conventional doppler modes have a difficult time capturing. It is used for small vessels, kidneys, and the brain. Although it has become more common in newer ultrasound systems, not all ultrasound machines employ power doppler options
عدل سابقا من قبل د.كمال سيد في الخميس مايو 30, 2024 12:14 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: General principles of US Physics موضوع: General principles of US Physics  الأربعاء مايو 29, 2024 1:36 pm الأربعاء مايو 29, 2024 1:36 pm | |
| general introducion
basics of US technique
Revision of principles of US physics, normal sonographic anatomy, in addition to pathology & most important US definitions
important definitions
1. Grey scale : is a display mode in which echo intensity is recorded as degrees of brightness or shades of grey. US image formation depends on the1/ the strength of the returning echoes & 2/Go Return Time.
So a strong echo will give a very bright image; a week echo gives a grey image; if NO echoes yields a black image.
Any area of US which produces echoes is called Echogenic
if an area produces NO echoes (echofree = No US echoes returning back to TXR) is called Anechoic compared to the surrounding
if an area produces less echoes is termed Hypoechoic
Hyperechoic is an area of US producing more echoes
Isoechoic is an area of US which produce same echoes compared to surrounding e.g pancreas is isoechoic to liver parenchyma.
Homogeneous & Heterogeneous are related to the overall distribution of the echo.
if echoe is equally distributed it gives a homogeneous echo texture
if echo is non equally distributed giving a heterogeneous echotexture e.g cirrhotic liver.
Standards & Guidelines to follow in scanning technique :
1.Perform thorough methodical surveys of structures in at least in two scanning planes
2.rule out normal variants
3. rule out pathology
4.US is real- time scanning & is operator dependent, SO take US images every 1 or 2 cm through a structure (a slow motion with the probe), & try to cover the whole structure or area of interest & NOT to miss any area of the organ under examination.
Documented AOI must be must be represented in at least 2 scanning planes (sagittal & transverse).
Always practice a professional & courteous behaviour with pt, keep their privacy, put them at ease & make them as comfortable as possible with pillows under the head & cover them properly.
Ask pt about his c/o, previous history, any surgery e.g GB removal (to spare time searching for GB), or any medication.
Make sure this is the correct pt with full 4 characters name.
Assist pt with any medical device attached to him e.g ECG monitor or foley's catheter.
Be familiar with sterile procedures, e.g in open wound areas or in intracavitory probes
Explain the procedure to pt using local languages
Select proper probe.
select scan type from preset menue.
Set depth, overall gain, TGC correctly
Put the focus at the level of AOI & on the area under examination
Basic US modes
There is M- mode {motion mode} for measuring heart rate
B-mode {brightness mode}
2D mode grey scale
Color Doppler or color flow imaging (CD) {CFI},
CW Doppler {continuos wave doppler}, PW Doppler {Power doppler},
When activate CD knob yu get 1/color in the image 2/ color map which shows the direction flow & 3/ color box 4/ color gain
Activate PD knob to get PW which is very sensitive to show smaller vessels & small flow
The following information should be include in the scan print :1/ pt name 2/ pt ID No. 3/ date & time, scanning site 4/(name of hospital or private office)5/ labeling of pathology in the area of interest (AOI) with measurements on one side of the print 6/ Name or initials of scanning person 7/ TXR frequency MHz 8/ pt position 9/ Area of interest 10/ scanning plane.
Selecting the the correct TXR for the AOI helps good interpretation & diagnosis.
set contrast & adjust the field size (TGC & overall gain) to best view the AOI near & far fild gain settings So that borders are well defined
document accurate images for diagnostic interpretation
set Depth, near, far & overall gain settings to enhance visualization of the AOI
Scanning planes : hold probe the correct way to ensure that the orientation marker of TXR (indicator) to be on the L top side of the screen.
1/ Sagittal plane : divides the body into equal L & RT sections
the TXR marker should point to the pt head
2/ Transverse {Axial}: divides body into equal upper (superior) & lower (inferior) sections.
in transverse scanning the marker should be to the pt RT side (to the operator LT side)
3/ Coronal plane divides body into anterior & posterior sections
the marker will point towards pt head.
Scanning planes are used to establish 1/ the direction that the US beam enters the body & 2/ the anatomic portion of anatomy being visualized from that particular direction
Anatomic areas seen on a sagittal scan :
1/ On anterior or posterior approach : US starts from anterior abdominal wall & returns back to TXR (with marker towards pt head), four anatomical areas appear on the screen: Anterior, posterior, superior & inferior
The anatomical area seen depends on probe position & the marker direction. The nearest anatomical area to probe is in the top of the screen, i.e anterior, with the posterior anatomic area being in the opposite far direction
As the marker is pointing towards pt head, the 3rd anatomical area (superior) will be to the Left of the operator, & 4th anatomical area (Inferior) will be to the RT of the operator in the opposite direction.
Anatomic areas seen on a transverse scan :
On anterior or posterior approach
(anterior, posterior, RT lateral & LT lateral)
in transverse scanning, the marker will always be towards pt RT side {operator LT side} which is (RT lateral anatomic area), while the opposite direction (pt LT side) {operator RT side} is the LT lateral anatomic area
BUT the anterior & posterior is the same as in sagittal scan
Anatomic areas seen on a transverse scan :
the approach will be RT lateral OR LT lateral
So the four anatomical areas in the screen will be 1/LT lateral/RT lateral 2/Medial 3/Superior 4/Inferior
the probe marker points towards the pt head, So there is a superior & an Inferior anatomical scan planes.
the nearest area to the probe is the lateral of the pt (RT OR LT), which will show on the top of the screen; and the area away from the lateral will be the medial anatomic area.
So the upper pole (superior) of the kidney will be on the RT of the pt towards the pt head, while the inferior pole is on the LT of the pt towards the feet.
Criteria to follow when scanning
1/ Always use a scanning couplant such as scanning gel
2/ Scan according to the lie of the organ, scanning plane may therefore be oblique, e.g length of the kidney; also in pancreatic measurements, probe must be transverse; also as the uterus is deviated to the RT side, so probe is put sagittal with a RT deviation.
3/ To better evaluate a structure, slightly Rock & slide the TXR while scanning
Scanning method
1/ Different TXR positions are used according to the AOI being evaluated, e.g we use subcostal, intercostal & oblique in abdomen scanning; in pelvic scanning, put probe above symphysis pubis, then angle downwards & upwards
2/ The best image aquisition is when probe is put perpendicular to AOI (probe straight up & down) to the scanning surface. Advantages of perpendicular scanning : A/ there will be maximum reflection B/ No any refraction artifact (e.g doubling of structure, edge shadow etc..)
3/ TXR may be Angled superiorly, inferiorly, or RT & LT laterally at varying degrees
4/ Subcostal scanning, with angling probe superiorly just beneath the inferior costal margin
5/ Intercostal scanning to scan the liver, by positioning probe between the ribs. It can be perpendicular, angled or subcostal
5/ Rotation : probe is rotated varying degrees to oblique the scanning plane
6/ Differnt pt positions can be used depending on the AOI being evaluated
عدل سابقا من قبل د.كمال سيد في الجمعة مايو 31, 2024 4:46 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: general principles of us physics موضوع: general principles of us physics  الجمعة مايو 31, 2024 1:18 pm الجمعة مايو 31, 2024 1:18 pm | |
| general principles of us physics
important definitions
1. Grey scale : is a display mode in which echo intensity is recorded as degrees of brightness or shades of grey. US image formation depends on the1/ the strength of the returning echoes & 2/Go Return Time.
So a strong echo will give a very bright image; a week echo gives a grey image; if NO echoes yields a black image.
Any area of US which produces echoes is called Echogenic
if an area produces NO echoes (echofree = No US echoes returning back to TXR) is called Anechoic compared to the surrounding
if an area produces less echoes is termed Hypoechoic
Hyperechoic is an area of US producing more echoes
Isoechoic is an area of US which produce same echoes compared to surrounding e.g pancreas is isoechoic to liver parenchyma.
Homogeneous & Heterogeneous are related to the overall distribution of the echo.
if echoe is equally distributed it gives a homogeneous echo texture
if echo is non equally distributed giving a heterogeneous echotexture e.g cirrhotic liver.
Standards & Guidelines to follow in scanning technique :
1.Perform thorough methodical surveys of structures in at least in two scanning planes
2.rule out normal variants
3. rule out pathology
4.US is real- time scanning & is operator dependent, SO take US images every 1 or 2 cm through a structure (a slow motion with the probe), & try to cover the whole structure or area of interest & NOT to miss any area of the organ under examination.
Documented AOI must be must be represented in at least 2 scanning planes (sagittal & transverse).
Always practice a professional & courteous behaviour with pt, keep their privacy, put them at ease & make them as comfortable as possible with pillows under the head & cover them properly.
Ask pt about his c/o, previous history, any surgery e.g GB removal (to spare time searching for GB), or any medication.
Make sure this is the correct pt with full 4 characters name.
Assist pt with any medical device attached to him e.g ECG monitor or foley's catheter.
Be familiar with sterile procedures, e.g in open wound areas or in intracavitory probes
Explain the procedure to pt using local languages
Select proper probe.
select scan type from preset menue.
Set depth, overall gain, TGC correctly
Put the focus at the level of AOI & on the area under examination
…
عدل سابقا من قبل د.كمال سيد في الجمعة مايو 31, 2024 6:30 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: general principles of us physics موضوع: general principles of us physics  الجمعة مايو 31, 2024 1:19 pm الجمعة مايو 31, 2024 1:19 pm | |
| Basic US modes
There is M- mode {motion mode} for measuring heart rate
B-mode {brightness mode}
2D mode grey scale
Color Doppler or color flow imaging (CD) {CFI},
CW Doppler {continuos wave doppler}, PW Doppler {Power doppler},
When activate CD knob yu get 1/color in the image 2/ color map which shows the direction flow & 3/ color box 4/ color gain
Activate PD knob to get PW which is very sensitive to show smaller vessels & small flow
The following information should be include in the scan print :1/ pt name 2/ pt ID No. 3/ date & time, scanning site 4/(name of hospital or private office)5/ labeling of pathology in the area of interest (AOI) with measurements on one side of the print 6/ Name or initials of scanning person 7/ TXR frequency MHz 8/ pt position 9/ Area of interest 10/ scanning plane.
Selecting the the correct TXR for the AOI helps good interpretation & diagnosis.
set contrast & adjust the field size (TGC & overall gain) to best view the AOI near & far fild gain settings So that borders are well defined
document accurate images for diagnostic interpretation
set Depth, near, far & overall gain settings to enhance visualization of the AOI
Scanning planes : hold probe the correct way to ensure that the orientation marker of TXR (indicator) to be on the L top side of the screen.
1/ Sagittal plane : divides the body into equal L & RT sections
the TXR marker should point to the pt head
2/ Transverse {Axial}: divides body into equal upper (superior) & lower (inferior) sections.
in transverse scanning the marker should be to the pt RT side (to the operator LT side)
3/ Coronal plane divides body into anterior & posterior sections
the marker will point towards pt head.
Scanning planes are used to establish 1/ the direction that the US beam enters the body & 2/ the anatomic portion of anatomy being visualized from that particular direction
Anatomic areas seen on a sagittal scan :
1/ On anterior or posterior approach : US starts from anterior abdominal wall & returns back to TXR (with marker towards pt head), four anatomical areas appear on the screen: Anterior, posterior, superior & inferior
The anatomical area seen depends on probe position & the marker direction. The nearest anatomical area to probe is in the top of the screen, i.e anterior, with the posterior anatomic area being in the opposite far direction
As the marker is pointing towards pt head, the 3rd anatomical area (superior) will be to the Left of the operator, & 4th anatomical area (Inferior) will be to the RT of the operator in the opposite direction.
Anatomic areas seen on a transverse scan :
On anterior or posterior approach
(anterior, posterior, RT lateral & LT lateral)
in transverse scanning, the marker will always be towards pt RT side {operator LT side} which is (RT lateral anatomic area), while the opposite direction (pt LT side) {operator RT side} is the LT lateral anatomic area
BUT the anterior & posterior is the same as in sagittal scan
Anatomic areas seen on a transverse scan :
the approach will be RT lateral OR LT lateral
So the four anatomical areas in the screen will be 1/LT lateral/RT lateral 2/Medial 3/Superior 4/Inferior
the probe marker points towards the pt head, So there is a superior & an Inferior anatomical scan planes.
the nearest area to the probe is the lateral of the pt (RT OR LT), which will show on the top of the screen; and the area away from the lateral will be the medial anatomic area.
So the upper pole (superior) of the kidney will be on the RT of the pt towards the pt head, while the inferior pole is on the LT of the pt towards the feet.
Criteria to follow when scanning
1/ Always use a scanning couplant such as scanning gel
2/ Scan according to the lie of the organ, scanning plane may therefore be oblique, e.g length of the kidney; also in pancreatic measurements, probe must be transverse; also as the uterus is deviated to the RT side, so probe is put sagittal with a RT deviation.
3/ To better evaluate a structure, slightly Rock & slide the TXR while scanning
Scanning method
1/ Different TXR positions are used according to the AOI being evaluated, e.g we use subcostal, intercostal & oblique in abdomen scanning; in pelvic scanning, put probe above symphysis pubis, then angle downwards & upwards
2/ The best image aquisition is when probe is put perpendicular to AOI (probe straight up & down) to the scanning surface. Advantages of perpendicular scanning : A/ there will be maximum reflection B/ No any refraction artifact (e.g doubling of structure, edge shadow etc..)
3/ TXR may be Angled superiorly, inferiorly, or RT & LT laterally at varying degrees
4/ Subcostal scanning, with angling probe superiorly just beneath the inferior costal margin
5/ Intercostal scanning to scan the liver, by positioning probe between the ribs
It can be perpendicular, angled or subcostal
6/ Rotation : probe is rotated varying degrees to oblique the scanning plane
7/ Different pt positions can be used depending on the AOI being evaluated:
For GB, it is better to scan oblique, searching for small stones in the fundus or impacted in the neck
عدل سابقا من قبل د.كمال سيد في الجمعة مايو 31, 2024 5:05 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: general principles of us physics موضوع: general principles of us physics  الجمعة مايو 31, 2024 7:50 pm الجمعة مايو 31, 2024 7:50 pm | |
| Cardinal TXR manipulation/movements {Sliding, Tilting, Rotation, Rocking}
It is important to understand that by manipulating the US probe, wee primarily, manipulating the direction of the beam, & by changing the direction of the beam, slightly different US images of the same structures can be obtained.
These fundamental probe manipulation maneuvers are referred to as {P . A . R . T} which stand for Pressure, Allignment, Rotation,Tilt
Pressure : for normal scanning, light TXR pressure should be applied so that probe is nearer to the organ in this pressure is important in order TO:
* Separate structures
* push gas out of the field of view {FOV}
*Compress adipose tissue to A/improve penetration B/ improve image quality & C/ shortens the distance to the structure if interest, leading to D/ decreasing attenuation C/ and a better image
In vascular studies compression is applied to differentiate between veins {Normally compressible} & arteries.
* in female pelvis scanning, apply pressure to elicit the {Sliding Organ Sign}; normally on pressure by TVS probe, the ovary moves smoothly from the uterus; if NO movement, it means that it is pathological adhesion.
* compression is needed to push a bowel or an anatomical structure out of the way of an intended needle path in US guided biopsy.
N.B excessive pressure can cause pt discomfort
Allignment {Sliding} :
Is done to * move the TAS probe to find the best window OR to * move to a different area of the pelvis or abdomen in any direction.
The main goal of this maneuver is to* find the structure of interest & to* position it optimally on the screen for needle advancement in US guided biopsy.
direct your beam at RT angle to the needle so as to * see if the tip of the needle is in or out.
* Allignment is very useful for tracing the potential structure proximally & distally for better verification of pertinent anatomy during a {scout scan} i.e {The foregoing case and other information are for the practitioner's convenience and for general information purposes only.}
Rotation
Rotating the TXR between *12 & 9 O'clock {90 degrees counter clockwise turn}, that is to rotate probe from transverse to longitudinal i.e 90 degrees.
By continuous rotation of the probe of 90 degrees from it's initial position, one can* change the view of the structure from it's short axis to it's long axis & vice versa
Tilting
Tilting is *Angling the TXR from side to side, allowing *oblique planes in the same axis to come into view; example in prostate scan.
Several goals can be achieved by tilting the probe:
By tilting the probe, * you are sweeping the US beam in the particular direction desired, and * you can preview the whole structure by* sliding the probe in the opposite direction of the tilt.
By * tilting the probe, a true short axis view of the object can be obtained, the long axis of which is not perpendicular to the initial US beam plane.
By * tilting the probe out of the true axial view of the target, the image will * change as follows :
A/ the distance from the surface to the target will increase. B/ The shape of the target on the screen will be untrue {oval instead of round}.
By tilting, the beam direction will change, leading to mild change in shape of the pathology of interest (e.g from round to oval etc..), but it is expected & we have an explanation for it
Rocking
Rocking is to* press the probe towards the head & then towards the feet.
The probe in a given plane of section allows * centering of an organ, structure or an AOI ; example especially in vascular, muscles, abdomen, & echocardiography.
Rocking will change the beam direction from side to side leading to covering & scanning of different areas
عدل سابقا من قبل د.كمال سيد في السبت يونيو 01, 2024 11:02 am عدل 1 مرات | |
|   | | | | Doppler US |  |
|
مواضيع مماثلة |  |
|
| | صلاحيات هذا المنتدى: | لاتستطيع الرد على المواضيع في هذا المنتدى
| |
| |
| |
|


