
موقع د. كمال سيد الدراوي
طبي_ اكاديمي _ ثقافي _ تعليمي _ _ استشارات طبية_فيديو طبي
|
|
| | UTERUS & OVARIES |  |
| | |
| كاتب الموضوع | رسالة |
|---|
د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: uterine positions موضوع: uterine positions  السبت يوليو 13, 2024 1:43 pm السبت يوليو 13, 2024 1:43 pm | |
| Uterine positions
*Version refers to the angle of the cx
*Flexion refers to the uterine body angle
1/ Anteverted Uterus
* The most A/common uterine position in which the B/CX faces or tilts anteriorly & there is C/NO bending of the body of the uterus, that is why we don't comment on it
2/ Retroverted uterus
* The A/CX is facing posteriorly (downwards) & there is B/NO noticeable bending of the body of the uterus
3/ Anteflexed uterus
* The body of the uterus will A/face anteriorly & there B/will be a bend b/w the lower part of the uterine body & the CX. the bend is B/facing anteriorly towards the UB
4/ Retroflexed uterus
* There will be A/a bend in the uterine body causing an angle which B/will face posteriorly away from the UB
In retroflexed position, the fundus of the body will appear on the RT side of the image
5/ Anteverted Anteflexed uterus
* The CX is A/facing anteriorly (upwards). Also the B/body of the uterus is bending upwards (anteriorly)
* the fundus is on the LT side of the image because it is bent facing anteriorly & the CX is also facing upwards
6/ Anteverted Retroflexed uterus
The CX is again facing upwards anteriorly, & the body of the uterus is bending away from UB, that is posteriorly
7/ In Retroverted & retroflexed position, the CX is tilted posteriorly, & the body of the uterus is also facing posteriorly, & will be seen on the RT side of the image because the UB will be appearing on the top LT side of the image
عدل سابقا من قبل د.كمال سيد في السبت يوليو 13, 2024 5:12 pm عدل 1 مرات | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: uterine positions موضوع: uterine positions  السبت يوليو 13, 2024 1:45 pm السبت يوليو 13, 2024 1:45 pm | |
| | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: US Evaluation of the Uterus موضوع: US Evaluation of the Uterus  الثلاثاء يوليو 30, 2024 12:20 pm الثلاثاء يوليو 30, 2024 12:20 pm | |
| Ultrasound Evaluation of the Uterus Outline
Imaging, 847
Guidelines, 847
Techniques, 847
Anatomy, 848
Congenital Malformations, 852
Benign Uterine Conditions, 857
Adenomyosis, 857
Leiomyomas, 858
Lipomatous Uterine Tumors, 866
Malignant Conditions, 866
Gestational Trophoblastic Disease, 866
Uterine Sarcomas, 868
Iatrogenic Processes, 871
Arteriovenous Malformations, 871
Intrauterine Contraceptive Devices, 872
The Postpartum and Postabortive Uterus, 872
Cervical Cysts and Polyps, 878
Conclusions, 878Summary of Key PointsSonography is the imaging modality of choice for evaluation of the myometrium, with magnetic resonance imaging (MRI) reserved as a problem-solving technique.
Many müllerian duct anomalies can be accurately diagnosed with sonography, and three-dimensional (3D) imaging of the fundal contour is diagnostic in differentiating the bicornuate uterus (>1 cm fundal cleft between the two horns) and the septate uterus.
Adenomyosis presents most commonly in middle-aged multiparous women with uterine tenderness, dysmenorrhea, and menorrhagia and most commonly appears on US images as an ill-defined or poorly marginated area within the myometrium or thickening of the hypoechoic subendometrial halo. The most specific findings are myometrial cysts and echogenic linear or nodular extension of the endometrium into the subjacent myometrium.
Leiomyoma (uterine fibrpid) is the most common uterine neoplasm. Symptoms are primarily related to location and size. Although most leiomyomas are A/ sharply marginated, B/ well-circumscribed, C/ hypoechoic masses, leiomyomas D/ may be isoechoic or echogenic relative to the myometrium.
There is overlap in the sonographic and MRI appearance of leiomyomas and
adenomyosis/adenomyomas, and the entities may coexist.
Lipoleiomyomas are typically A/ extremely echogenic and B/ sharply marginated with
C/ posterior attenuation.
Leiomyosarcomas may be difficult to differentiate from degenerating leiomyomas on both sonography and MRI.
Patients with gestational trophoblastic disease (GTD) most commonly present with an A/ echogenic endometrial mass containing C/ numerous small cysts and D/ demonstrating increased vascularity. Fetal parts may be seen in partial moles or coexistent twin pregnancy. Myometrial invasion can be seen with A/ persistent disease or B/ choriocarcinomas, but on imaging may be C/ difficult to differentiate from increased vascularity and “pseudoinvasion” from the placental bed, arteriovenous malformations (AVMs), or retained products of conception (RPOC).
Uterine AVMs are most often A/ traumatic in origin but may also be B/ congenital or diagnosed in the setting of C/ persistent GTD D/ and RPOC. .
Sonography may be helpful in the diagnosis of endocervical polyps.
However, the sonographic appearances of cervical leiomyoma and carcinoma overlap
Sonography is clearly the modality of choice for imaging the female pelvis, including the uterus and adnexal structures. In our clinical laboratory, a combination of transabdominal pelvic scanning as well as transvaginal examination is performed in most patients. This approach allows the examiner to evaluate the true pelvis in its entirety with a wide field of view on transabdominal imaging, as well as to assess specific structures using high-resolution images obtained on transvaginal scanning. Primary evaluation with US in conjunction with clinical information is often sufficient for diagnosis and patient management and will help optimize recommendations for further imaging as necessary. When US evaluation fails to provide adequate information or does not answer the clinical question, further evaluation with MRI, computed tomography (CT), scanning, hysterography, or saline infusion sonography (SIS) can be performed. MRI of the uterus is discussed in detail in Chapter 36 . In this chapter, we discuss US evaluation of the normal uterus, anatomic variants, and benign and malignant conditions. A discussion of the normal and abnormal endometrium in the patient who presents with abnormal uterine bleeding is presented in Chapter 27 .
https://radiologykey.com/ultrasound-evaluation-of-the-uterus-2/
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: imaging guidelines موضوع: imaging guidelines  الثلاثاء يوليو 30, 2024 6:16 pm الثلاثاء يوليو 30, 2024 6:16 pm | |
| The uterus is a pear-shaped organ in the reproductive system
of female
It’s where a fertilized egg implants during pregnancy and where your baby
develops till birth
Inferiorly, the uterine corpus continues with the cervix. The upper uterine portion is called the fundus, on either side of which the fallopian tubes originate.The uterus is located between the urinary bladder anteriorly and the rectum posteriorly. The average dimensions of the uterus in an adult female are 8 cm long, 5 cm across, and 4 cm thick. The uterine cavity has an average volume of 80 mL to 200 mL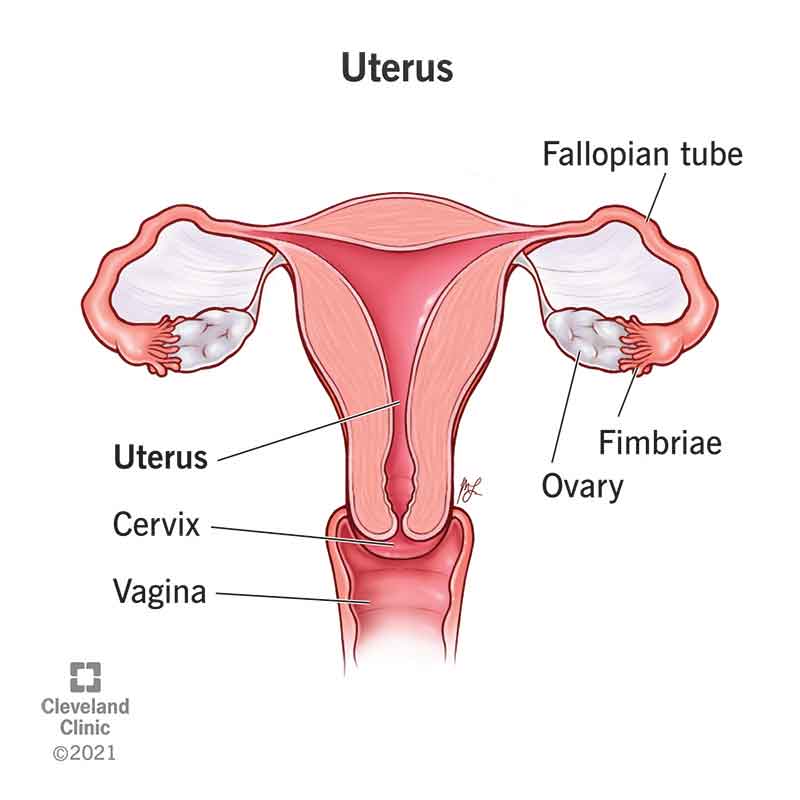 Imaging
Guidelines
The American Institute of US in Medicine (AIUM) guidelines for imaging of the uterus have been developed to assist physicians in performing sonographic studies of the female pelvis. Knowing the potential, but also the limitations, of US helps us to maximize the probability of detecting most significant abnormalities. As with any clinical test, US examination of the pelvis should be performed only if there is a valid clinical reason. Following the AIUM guidelines, the indications for pelvic sonography include, but are not limited to, the following:Evaluation of pelvic pain Evaluation of pelvic masses Evaluation of endocrine abnormalities, including polycystic ovaries Evaluation of dysmenorrhea (painful menses) Evaluation of amenorrhea Evaluation of abnormal bleeding Evaluation of delayed menses Follow-up of a previously detected abnormality Evaluation, monitoring, and/or treatment of infertility patients Evaluation in the presence of a limited clinical examination of the pelvis Evaluation for signs or symptoms of pelvic infection Further characterization of a pelvic abnormality noted on another imaging study Evaluation of congenital uterine and lower genital tract anomalies Evaluation of excessive bleeding, pain, or signs of infection after pelvic surgery, delivery, or abortion Localization of an intrauterine contraceptive device Screening for malignancy in high-risk patients Evaluation of incontinence or pelvic organ prolapse Guidance for interventional or surgical procedures; and Preoperative and postoperative evaluation of pelvic structuresTechniques
All relevant anatomic structures in the pelvis should be identified first by transabdominal technique, and then more detailed evaluation of the deep pelvic structures should be performed using the transvaginal (TVS) technique. In specific situations when transvaginal evaluation cannot be performed or tolerated, transrectal (TRS) or transperineal (TPS) evaluation can be very useful.The transducer (TXR) should be selected to operate at the A/ highest clinically appropriate frequency that will allow adequate visualization of deep pelvic structures. For transabdominal B/ (TAS) evaluation, C/ a *3.5-MHz or higher transducer is employed. A *Curved linear array TXRs, as well as *sector TXRs with a smaller footprint, are most often employed. For TAS evaluation, C/ the UB should be adequately distended to *displace bowel superiorly out of the true pelvis and *to provide an acoustic window to visualize the uterus and adnexa ( Fig. 28-1 ). 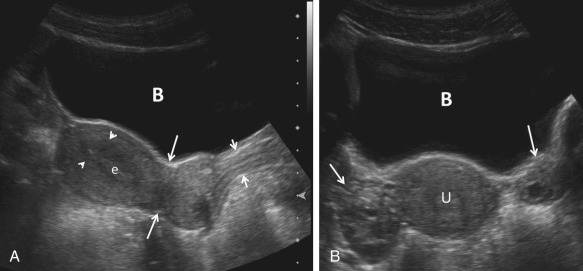 FIG 28-1Transabdominal gray-scale ultrasound images of the normal uterus. A, Sagittal imaging plane. Note indentation below the lower uterine segment indicating the level of the internal os ( long arrows ), the striated appearance of the vagina ( short arrows ), the linear homogeneously echogenic endometrium (e), and the surrounding hypoechoic subendometrial halo ( arrowheads ). Note the acoustic window provided by the distended urinary bladder (B). B, Transverse imaging plane. Note the bladder (B), right and left ovaries ( arrows ), and uterus (U).For TVS evaluation, A/ the urinary bladder (UB) should be emptied and the patient B/ placed in a comfortable position but with her C/ pelvis tilted either with the use of stirrups or by the placement of padding under the patient to D/ elevate the hips. The patient OR the sonographer, depending upon the patient’s preference, may introduce the vaginal TXR with real-time monitoring. For TVS evaluation, the AIUM recommends using probe frequencies of 5 MHz or higher (Fig. 28-2). If E/ a male sonologist is performing the examination, a female member of the staff should be present as a chaperone (companion/superviser). However, in some clinical situations, a chaperone is helpful and recommended even for a female sonologist. FIG 28-1Transabdominal gray-scale ultrasound images of the normal uterus. A, Sagittal imaging plane. Note indentation below the lower uterine segment indicating the level of the internal os ( long arrows ), the striated appearance of the vagina ( short arrows ), the linear homogeneously echogenic endometrium (e), and the surrounding hypoechoic subendometrial halo ( arrowheads ). Note the acoustic window provided by the distended urinary bladder (B). B, Transverse imaging plane. Note the bladder (B), right and left ovaries ( arrows ), and uterus (U).For TVS evaluation, A/ the urinary bladder (UB) should be emptied and the patient B/ placed in a comfortable position but with her C/ pelvis tilted either with the use of stirrups or by the placement of padding under the patient to D/ elevate the hips. The patient OR the sonographer, depending upon the patient’s preference, may introduce the vaginal TXR with real-time monitoring. For TVS evaluation, the AIUM recommends using probe frequencies of 5 MHz or higher (Fig. 28-2). If E/ a male sonologist is performing the examination, a female member of the staff should be present as a chaperone (companion/superviser). However, in some clinical situations, a chaperone is helpful and recommended even for a female sonologist.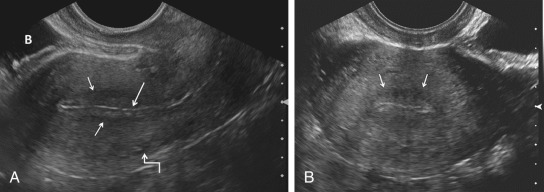 FIG 28-2Transvaginal (TVS) gray-scale US images of the normal uterus. A, Sagittal imaging plane. Note thin brightly echogenic line ( long arrow ) representing artifact or mucus between the echogenic anterior and posterior layers of the endometrium and the subjacent hypoechoic subendometrial halo ( short arrows ). The anechoic tubular arcuate vessels separating the outer from the intermediate layer of the myometrium are faintly visualized ( crooked arrow ). B, bladder. B, Transverse imaging plane. The hypoechoic subendometrial halo ( arrows ) can be seen surrounding the echogenic endometrium. Note significantly improved resolution and visualization of the normal zonal anatomy in these higher frequency transvaginal images in comparison to the lower frequency transabdominal images ( Fig. 28-1 ). However, the transabdominal images have a larger field of view, providing a better overview of pelvic structures. The vagina, uterus, and the UB are used as reference points for identification of the remaining normal and abnormal pelvic structures. The uterine 1. size, 2. shape, and 3. orientation should be assessed and documented in both sagittal (long-axis) and transverse (axial or short-axis) planes. The 4. endometrium, 5. myometrium, and 6. cervix should be carefully evaluated, and 7. their appearance documented. The uterine 8. length is measured in A/ long axis (sagittal) from the fundus to the external os of the cervix, and the B/ anteroposterior (AP) dimension is measured on the same image perpendicular to the FIG 28-2Transvaginal (TVS) gray-scale US images of the normal uterus. A, Sagittal imaging plane. Note thin brightly echogenic line ( long arrow ) representing artifact or mucus between the echogenic anterior and posterior layers of the endometrium and the subjacent hypoechoic subendometrial halo ( short arrows ). The anechoic tubular arcuate vessels separating the outer from the intermediate layer of the myometrium are faintly visualized ( crooked arrow ). B, bladder. B, Transverse imaging plane. The hypoechoic subendometrial halo ( arrows ) can be seen surrounding the echogenic endometrium. Note significantly improved resolution and visualization of the normal zonal anatomy in these higher frequency transvaginal images in comparison to the lower frequency transabdominal images ( Fig. 28-1 ). However, the transabdominal images have a larger field of view, providing a better overview of pelvic structures. The vagina, uterus, and the UB are used as reference points for identification of the remaining normal and abnormal pelvic structures. The uterine 1. size, 2. shape, and 3. orientation should be assessed and documented in both sagittal (long-axis) and transverse (axial or short-axis) planes. The 4. endometrium, 5. myometrium, and 6. cervix should be carefully evaluated, and 7. their appearance documented. The uterine 8. length is measured in A/ long axis (sagittal) from the fundus to the external os of the cervix, and the B/ anteroposterior (AP) dimension is measured on the same image perpendicular to the
long axis. The C/ width is measured on either a transaxial or coronal imaging plane. If the 10. volume of the uterine corpus is assessed, the cervical component should be excluded. Myometrial A/ masses and B/ contour abnormalities should be recorded in two different planes and their C/ locations recorded. Assessment of the endometrium is performed A/ primarily in the sagittal (sometimes coronal) plane. B/ Variations of the normal appearance of the endometrium during different phases of the menstrual cycle and with hormonal supplementation should be considered (Fig. 28-3) 11.Doppler C/ evaluation of the uterus and endometrium can be of added value
12. 3D imaging is increasingly available and can also provide valuable additional information, particularly by providing a coronal image of the fundal contour of the uterus in women with suspected uterine congenital malformations and to localize leiomyomas.NEXThttps://radiologykey.com/ultrasound-evaluation-of-the-uterus-2/
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: US Evaluation of the Uterus موضوع: US Evaluation of the Uterus  الثلاثاء يوليو 30, 2024 6:55 pm الثلاثاء يوليو 30, 2024 6:55 pm | |
| US Evaluation of the Uterus contd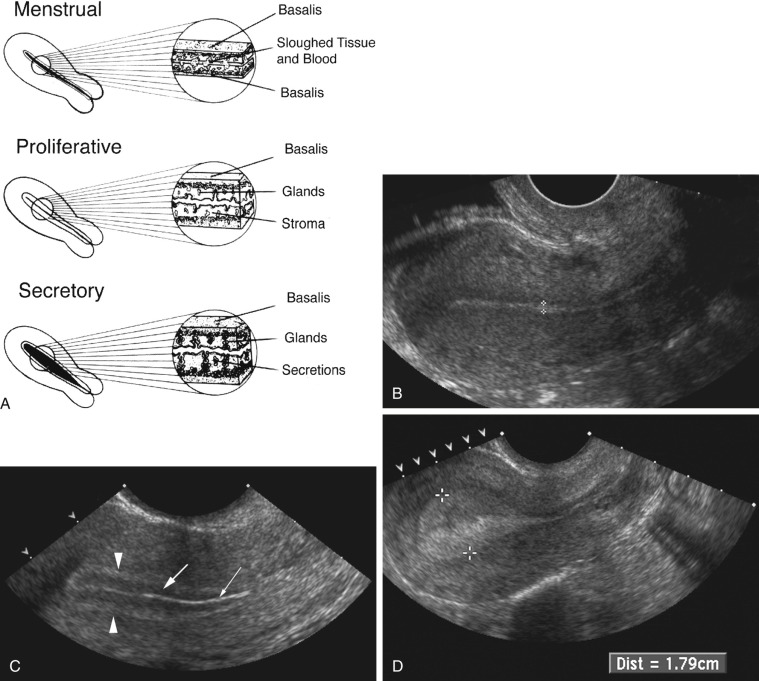 FIG 28-3 A, Diagram depicting normal development of the endometrium during the menstrual, proliferative, and secretory phases. In the menstrual phase, the endometrium appears as a thin, irregular interface. The central echogenicity probably arises from sloughed tissue and blood. In the proliferative phase, the endometrium is relatively hypoechoic, likely a reflection of the straight and orderly arrangement of the glandular elements. The central thin, echogenic line is likely a specular reflection from the endometrial surfaces. In the secretory phase, the endometrium achieves its maximum thickness and echogenicity. This appearance is from the distended and tortuous glands, which contain secretions. B, Postmenstrual transvaginal sagittal image of the uterus demonstrating the normal thin homogeneously echogenic early proliferative endometrium ( calipers ). FIG 28-3 A, Diagram depicting normal development of the endometrium during the menstrual, proliferative, and secretory phases. In the menstrual phase, the endometrium appears as a thin, irregular interface. The central echogenicity probably arises from sloughed tissue and blood. In the proliferative phase, the endometrium is relatively hypoechoic, likely a reflection of the straight and orderly arrangement of the glandular elements. The central thin, echogenic line is likely a specular reflection from the endometrial surfaces. In the secretory phase, the endometrium achieves its maximum thickness and echogenicity. This appearance is from the distended and tortuous glands, which contain secretions. B, Postmenstrual transvaginal sagittal image of the uterus demonstrating the normal thin homogeneously echogenic early proliferative endometrium ( calipers ).
C, Transvaginal sagittal image of the periovulatory endometrium. A three-layered endometrium is seen, giving the endometrium a striated appearance: the collapsed endometrial lumen is demonstrated by the very thin central echogenic line ( thin arrow ). The surrounding hypoechoic layer representing the edematous functionalis endometrium ( thick arrow ) and an outer hyperechoic layer representing the basal endometrium ( arrowheads ) are seen. D, Transvaginal sagittal image of the secretory endometrium. In the secretory stage of the menstrual cycle, the endometrium ( calipers ) becomes thick and more homogeneously echogenic. SIS, or as it is often referred to, sonohysterography, is an innovative technique used to evaluate a variety of endometrial and myometrial processes that involve the endometrial canal. The most common indications for SIS include, but are not limited to, evaluation of the following: Abnormal uterine bleeding
Uterine cavity, especially with regard to uterine leiomyomas, polyps, and synechiae
Abnormalities detected on transvaginal sonography, including focal or diffuse endometrial or intracavitary abnormalities
Congenital abnormalities of the uterus
Infertility
Recurrent pregnancy loss
SIS is contraindicated in women who could be pregnant or have an active infection. Because the normal secretory endometrium may be thick and simulate endometrial disease, the examination should be scheduled in premenopausal women during the follicular phase of the menstrual cycle, after menstrual flow has ceased but prior to ovulation, no later than the 10th day of the menstrual cycle. Active vaginal bleeding is not generally a contraindication but can make imaging challenging or even nondiagnostic. At our institution, we perform a preliminary transabdominal and transvaginal sonogram before SIS. After the procedure is explained to the patient, the external os is cleansed before catheterization of the cervical canal using aseptic technique. A sonohysterography catheter, flushed with saline to remove any air
bubbles is then advanced into the endometrial canal . Once in the endometrial canal, the balloon is inflated (preferably with saline rather than air to avoid shadowing) so that the catheter does not become dislodged. However, some clinicians prefer to use a catheter without a balloon. The speculum is removed, and the transvaginal probe is reinserted adjacent to the catheter. Under ultrasound guidance, the balloon is gently retracted to occlude the internal os. Sterile saline should be administered under real-time sonography. The amount of saline introduced is variable, often between 5 and 30 mL. Normal anatomy and abnormal findings should be documented in two separate imaging planes using a high-frequency transvaginal probe, and the endometrium should be fully evaluated from one cornua to the other ( Fig. 28-4 ). Additional techniques such as color Doppler and 3D imaging may be helpful in evaluating both normal and abnormal findings. 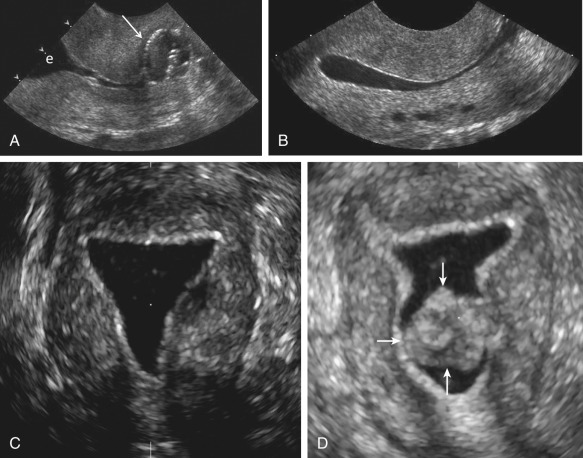 FIG 28-4 Saline-infused sonohysterogram. A, Transvaginal sagittal image of the cervix demonstrating the catheter balloon (arrow) positioned in the lower endocervical canal. Anechoic fluid is in the upper endocervical canal and lower endometrial cavity (e). B, Transvaginal sagittal image after saline infusion. The normal thin echogenic endometrium is well seen circumferentially. The endometrial cavity is filled with anechoic fluid. Note several small, round anechoic structures in a linear configuration in the posterior wall of the myometrium. These are the arcuate vessels and would fill in with color Doppler. FIG 28-4 Saline-infused sonohysterogram. A, Transvaginal sagittal image of the cervix demonstrating the catheter balloon (arrow) positioned in the lower endocervical canal. Anechoic fluid is in the upper endocervical canal and lower endometrial cavity (e). B, Transvaginal sagittal image after saline infusion. The normal thin echogenic endometrium is well seen circumferentially. The endometrial cavity is filled with anechoic fluid. Note several small, round anechoic structures in a linear configuration in the posterior wall of the myometrium. These are the arcuate vessels and would fill in with color Doppler.
C, A coronal three-dimensional reconstruction after saline infusion, demonstrating the normal regular, thin, echogenic endometrium without any intracavitary abnormalities. D, In comparison, a coronal three-dimensional reconstruction after saline infusion revealed a 100% intracavitary leiomyoma (arrows), separate from the thin, regular echogenic endometrium.https://radiologykey.com/ultrasound-evaluation-of-the-uterus-2/
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: US Evaluation of the Uterus موضوع: US Evaluation of the Uterus  الأربعاء يوليو 31, 2024 1:47 pm الأربعاء يوليو 31, 2024 1:47 pm | |
| US Evaluation of the Uterus contd
Anatomy The uterus is a hollow organ in which the myometrium is firmly adherent to a thin internal layer of endometrium. Externally the uterus is embedded between the two layers of the broad ligament. Anatomically, the uterus lies between the bladder anteriorly and the rectosigmoid colon posteriorly. The uterus is divided into two major parts, the body or (corpus) and the cervix. The most superior aspect of the uterus is referred to as the fundus, and the area where the fallopian tubes enter into the uterus is referred to as the cornua. Anterior to the fallopian tubes are the round ligaments, one on each side, which extend anterolaterally, coursing through the inguinal canals and inserting onto the fascia of the labia majora. The uterus has a dual arterial blood supply. The majority of the blood supply comes from the uterine arteries, which arise from the internal iliac arteries, and a minor source of blood supply is the ovarian arteries. The uterus is most often anteverted and anteflexed (Fig. 28-5), but it may also be retroflexed (Fig. 28-6) or retroverted (Fig. 28-7). Descriptions of flexion refer to the relationship of the body of the uterus to the cervix at the level of the internal os (usually the angle is about 270 degrees), whereas version refers to the cervical relationship to the vagina. The cervix of the uterus is fixed in the midline. However, the body of the uterus can be mobile, and uterine position and orientation may change with varying degrees of bladder and rectal distention. Retroversion and retroflexion are not infrequent in the nongravid state. In such cases the fundus of the uterus is positioned in the sacral hollow. During pregnancy the uterus enlarges and physiologically undergoes reduction by the 14th to 16th weeks of gestation. The fundus of the uterus then rises into the false pelvis. If this fails to happen, the uterus becomes “trapped” in the sacral hollow, often referred to as “incarcerated.” In cases of incarceration of the uterus, the cervix is drawn upward either against or above the symphysis pubis, resulting in distortion of the bladder and urethra as the gestation progresses. The posteriorly positioned fundus can cause pressure on the rectum. Typically, patients present between the 13th to 17th weeks of pregnancy with symptoms of bladder outlet obstruction. A history of multiple trips to the emergency room for bladder outlet obstruction should raise suspicion. 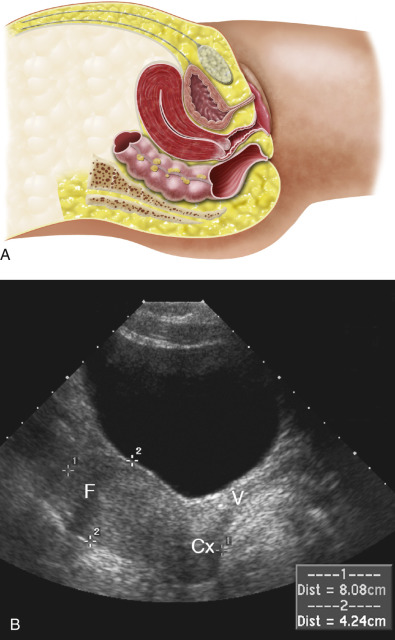 FIG 28-5 A, Illustration demonstrating an anteflexed, anteverted normal uterus. The cervix is pointing slightly more posterior in relationship to the vagina, and the fundus is flexed anterior in relation to the cervix. B, Midline sagittal sonogram demonstrating anteversion of the cervix (Cx) to the vagina (V). A distended urinary bladder slightly displaces the fundus (F) posteriorly. Standard measurements of the uterine size are made from fundus to cervix (calipers 1) and from anterior to posterior uterine wall (calipers 2) on sagittal transabdominal view. (A from James A. Cooper, MD, San Diego, CA.) 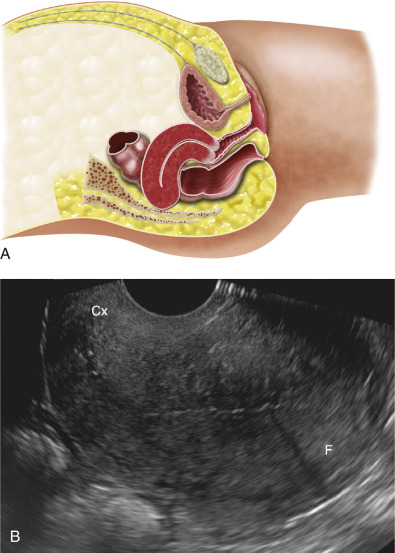 FIG 28-6 A, Illustration demonstrating a retroflexed uterus. The cervix is in conventional position in relationship to the vagina. However, the uterine fundus is flexed posteriorly at the level of the internal os in relation to the cervix. B, Midline sagittal transvaginal sonogram demonstrating uterine retroflexion. Uterine fundus (F) is positioned posterior and retroflexed in relation to the cervix (Cx). Note angulation between the echogenic endocervical canal and thin echogenic endometrium (owing to the flexion). (A from James A. Cooper, MD, San Diego, CA.) 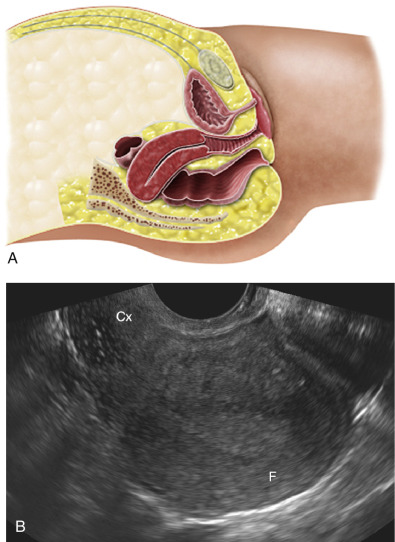 FIG 28-7 A, Illustration demonstrating a retroverted uterus; the cervix is angled slightly posterior in relation to the vagina, and the fundus is bent slightly posterior in relation to the cervix, indicating retroflexion as well. B, Midline sagittal transvaginal sonogram demonstrating posterior displacement of the fundus (F) and posterior angulation of the cervix (Cx). (A from James A. Cooper, MD, San Diego, CA.)
A constellation of three findings on sonography is diagnostic of an incarcerated uterus
The pregnancy is deep within the cul-de-sac.
The maternal urinary bladder lies anterior rather than inferior to the uterine corpus and marked bladder distention is noted.
A soft tissue structure (the cervix) is seen between the bladder and pregnancy. This appearance can be misconstrued as an empty uterus associated with an ectopic or abdominal pregnancy
Failure to recognize an incarcerated uterus can result in compromise of the uterine circulation, leading to spontaneous abortion or even uterine rupture. If recognized early, manual uterine repositioning is usually possible ( Fig. 28-8 ). 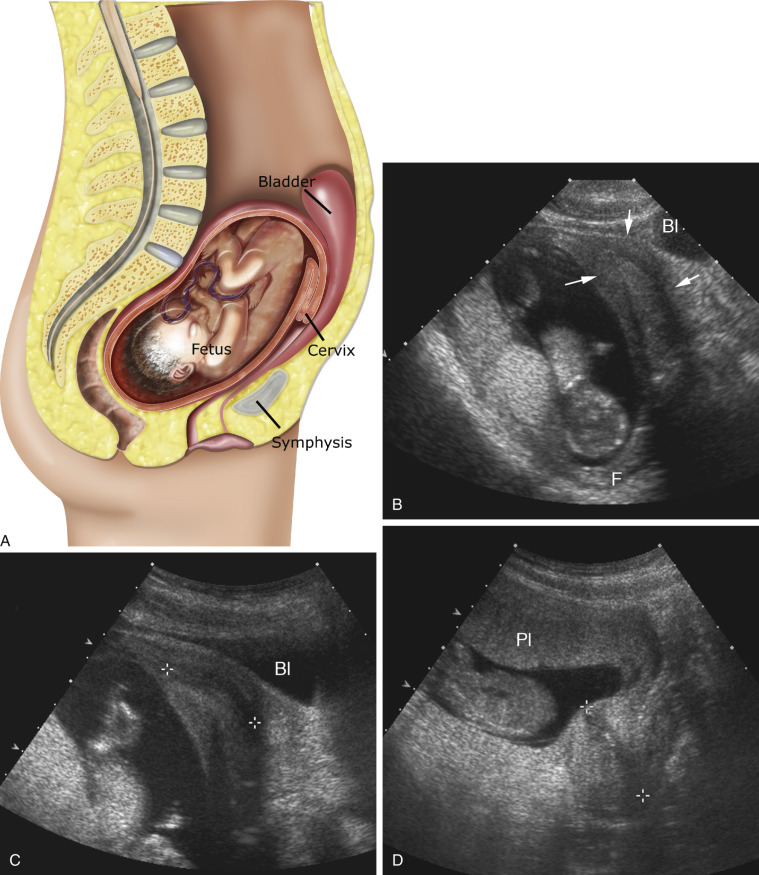 FIG 28-8 A, Illustration demonstrating an incarcerated uterus. If a retroflexed uterus fails to reduce and the gestation progresses, the fundus will become incarcerated deep in the pelvis within the sacral hollow. The cervix will be drawn anteriorly and superiorly and the bladder will be displaced superiorly. B, Transabdominal sagittal image of an incarcerated uterus in a patient with a 14-week-old gestation. The patient presented with inability to empty the urinary bladder. The uterine fundus (F) is trapped in the sacral hollow. The cervix ( arrows ) is drawn anteriorly and superiorly and can be misconstrued as an empty uterus, thereby suggesting an ectopic or transabdominal pregnancy. Bl, bladder. C, Sagittal view of the same patient demonstrating the degree to which the bladder (Bl) is drawn superiorly. Note abnormal position of the cervix ( calipers ). D, Following manual reduction, note normal physiologic relationship of the uterus and cervix ( calipers ). The placenta (Pl) is located anteriorly although it appeared posterior in location when the uterus was incarcerated. (A from James A. Cooper, MD, San Diego, CA.)https://radiologykey.com/ultrasound-evaluation-of-the-uterus-2/
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: US Evaluation of the Uterus موضوع: US Evaluation of the Uterus  الأربعاء يوليو 31, 2024 6:41 pm الأربعاء يوليو 31, 2024 6:41 pm | |
| The shape and size of the uterus vary throughout life, affected mostly by hormonal status. The mean measurement of the prepubertal uterus is 2.8 cm in length and 0.8 cm in maximum anteroposterior dimension, with the cervix accounting for two thirds of the total length and contributing to the pear-shaped appearance (Fig. 28-9). It is important to remember that in the immediate postdelivery state, the neonatal uterus can be slightly larger due to effects of residual maternal hormones. For the same reason, the echogenic endometrium is well seen and a small amount of fluid can be present in the endometrial cavity. 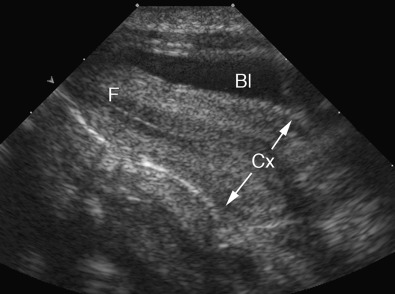 FIG 28-9 Transabdominal sagittal view of the normal prepubertal uterus. The cervix (Cx) is significantly more prominent than the body or fundus (F) of the uterus. Bl, bladder. From birth until 4 years, the uterus decreases in size. At approximately 8 years of age, uterus starts to grow preferentially in the fundus,The uterus continues to grow for several years after menarche until it reaches the mean dimensions of a reproductive age uterus, which are approximately 7cm long and 4 cm wide . Parity increases the size of the uterus, with a multiparous uterus measuring approximately 8.5 cm by 5.5 cm FIG 28-9 Transabdominal sagittal view of the normal prepubertal uterus. The cervix (Cx) is significantly more prominent than the body or fundus (F) of the uterus. Bl, bladder. From birth until 4 years, the uterus decreases in size. At approximately 8 years of age, uterus starts to grow preferentially in the fundus,The uterus continues to grow for several years after menarche until it reaches the mean dimensions of a reproductive age uterus, which are approximately 7cm long and 4 cm wide . Parity increases the size of the uterus, with a multiparous uterus measuring approximately 8.5 cm by 5.5 cm
Following menopause, the uterus decreases in size. The decrease in size is related to the number of years since menopause, although the reduction in size is believed to be most rapid during the first decade following menopause. The length of the normal postmenopausal uterus has been reported to range from 3.5 to 6.5 cm
and the anteroposterior dimension from 1.2 to 1.8 cm. The normal myometrium is composed of three layers : The innermost layer, A/immediately subjacent to the endometrium, B/is the thinnest and is
relatively compact C/histologically. This layer is also D/both hypovascular and hypoechoic when compared to the echogenic endometrium and surrounding middle layer of the myometrium. This layer is often referred to as the E/subendometrial halo and may not always be visualized sonographically. F/Sometimes, small
extremely echogenic foci, usually less than a few millimeters in size and without posterior shadowing, are seen in the inner myometrium at the endometrial/myometrial interface. These foci represent dystrophic calcifications due to previous intrauterine instrumentation and have no clinical significance. The middle or intermediate layer lies A/between the subendometrial halo and the arcuate vessels.
This is B/the thickest myometrial layer and is normally C/uniform and intermediate in echogenicity. The outer layer lies A/peripheral to or above the arcuate vessels. This layer is C/relatively thin and slightly D/less echogenic
compared to the intermediate layer in most patients. The cervix is A/measured from the internal os, identified by narrowing or “waisting” of the uterus at the junction of the lower uterine segment with the cervix to the lips of the external os, which can be seen to project into the lumen of the vagina.
B/The central endocervical canal is echogenic and continuous with the endometrium. The surrounding C/fibrous cervical stroma is quite hypoechoic and is continuous with the subendometrial halo, if present. The outer cervical muscular layer is D/continuous with and similar in
echogenicity to the intermediate layer of the myometrium (Fig. 28-10). 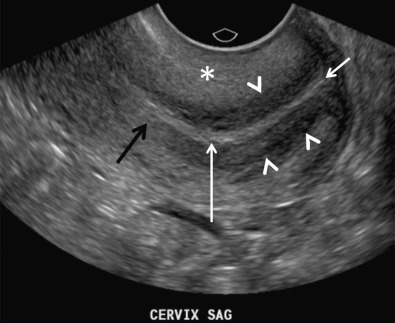 FIG 28-10 Normal sonographic zonal anatomy of the cervix. Note central linear echogenic endocervical canal (long white arrow), subjacent hypoechoic fibrous cervical stroma (arrowheads), outer muscular layer of intermediate echogenicity ( asterisk ), external os (short white arrow) between the lips of the cervix, and internal os (black arrow) at the level of narrowing or constriction between the body of the uterus and the cervix. The arcuate vessels separate the A/outer layer from the intermediate layer of the myometrium. FIG 28-10 Normal sonographic zonal anatomy of the cervix. Note central linear echogenic endocervical canal (long white arrow), subjacent hypoechoic fibrous cervical stroma (arrowheads), outer muscular layer of intermediate echogenicity ( asterisk ), external os (short white arrow) between the lips of the cervix, and internal os (black arrow) at the level of narrowing or constriction between the body of the uterus and the cervix. The arcuate vessels separate the A/outer layer from the intermediate layer of the myometrium.
The B/arcuate veins are larger than the arcuate arteries and are
C/potentially compressible with with excessive probe or manual pressure. The arcuate vessels (particularly the veins) can be D/prominent and mimic cystic changes. This potential misinterpretation can easily be clarified by using color Doppler imaging (Fig. 28-11). The arcuate E/arteries branch into radial arteries that F/penetrate the intermediate layer and G/reach the level of the inner layer. The arcuate arteries H/may calcify in postmenopausal women, and this process can be seen earlier in diabetic patients. This change is considered I/part of the normal aging process (Fig. 28-12). 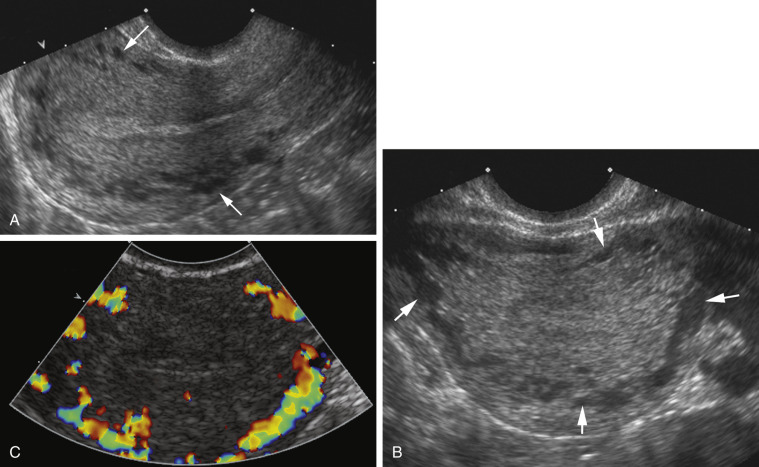 FIG 28-11 Transvaginal sagittal ( A ) and transverse ( B ) sonograms of the uterus demonstrating prominent anechoic round areas ( arrows ) between the outer third and inner myometrium. These are the arcuate vessels, which can mimic cystic changes. C, These cystic appearing spaces are confirmed to be arcuate vessels by applying color Doppler. FIG 28-11 Transvaginal sagittal ( A ) and transverse ( B ) sonograms of the uterus demonstrating prominent anechoic round areas ( arrows ) between the outer third and inner myometrium. These are the arcuate vessels, which can mimic cystic changes. C, These cystic appearing spaces are confirmed to be arcuate vessels by applying color Doppler. 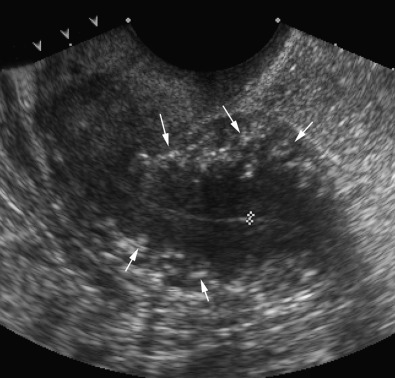 FIG 28-12 Transvaginal sagittal view of small retroverted and retroflexed uterus in a postmenopausal woman demonstrating arcuate artery calcifications (arrows). Calipers show the endometrium. https://radiologykey.com/ultrasound-evaluation-of-the-uterus-2/ FIG 28-12 Transvaginal sagittal view of small retroverted and retroflexed uterus in a postmenopausal woman demonstrating arcuate artery calcifications (arrows). Calipers show the endometrium. https://radiologykey.com/ultrasound-evaluation-of-the-uterus-2/
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: US Evaluation of the Uterus موضوع: US Evaluation of the Uterus  الخميس أغسطس 01, 2024 6:09 pm الخميس أغسطس 01, 2024 6:09 pm | |
| Congenital MalformationsThe incidence of congenital müllerian duct anomalies is estimated to be approximately 0.5% in the general population. However, they are more often diagnosed during workup for infertility, frequent miscarriages, or menstrual disorders. Embryologically, the two paired müllerian ducts ultimately develop into the fallopian tubes, uterus, cervix, and the upper two thirds to four fifths of the vagina. The lower one fifth to one third of the vagina and the ovaries have a separate embryologic origin. Uterine malformations arise from three different causes: 1.failure of development of the müllerian ducts, 2.failure of fusion of the müllerian ducts, 3.or failure of resorption of the median septum (Fig. 28-13). There is a strong association of upper urinary tract anomalies with congenital uterine malformations. These anomalies have been reported to be most common in patients with hypoplasia or agenesis, occurring in as many as 30% to 40% of patients. Ispilateral renal agenesis and ectopic pelvic kidney are most common.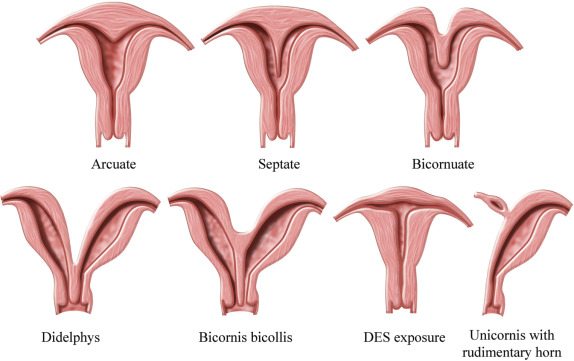 FIG 28-13 Most common uterine anomalies. DES, diethylstilbestrol. (Illustration by James A. Cooper, MD, San Diego, CA.) Early developmental failure of the müllerian ducts can result in agenesis or hypoplasia of the proximal two thirds of the vagina, cervix, and uterus, being part of the Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. This syndrome is an extreme form of müllerian duct anomaly with complete agenesis of the proximal vagina and anomalous cervix and uterus, and patients usually present in early puberty with primary amenorrhea. The ovaries are normal but the fallopian tubes may be closed and the uterus is often anomalous. The vaginal aplasia can vary from complete absence to a blind-ending pouch. Associated renal anomalies are common, in particular absence or ectopia of the kidney. Because there can be subtypes of MRKH syndrome as well as overlap with other rare müllerian duct hypoplasia/aplasia syndromes, it is important to describe findings rather than trying to fit them into a strict category. MRI is usually the most helpful imaging modality for diagnosis of this entity given the complex spectrum of findings. Most important, is communication with the clinical team regarding the relevance of findings and preoperative planning.Arrested development of the müllerian ducts can also cause uterine agenesis or hypoplasia. This abnormality may present as vaginal, cervical, fundal, tubal, or combined agenesis or hypoplasia.Complete or partial agenesis of a unilateral müllerian duct leads to development of a unicornuate uterus with a single fallopian tube (Fig. 28-13). The unicornuate uterus accounts for approximately 20% of all müllerian duct anomalies. In some cases, a rudimentary horn on the opposite side can be seen. This rudimentary horn may or may not communicate with the endometrial cavity in the normal side. If there is no communication between the endometrial cavities of the rudimentary and normal horns, retrograde menstruation may occur, leading to the development of endometriosis. Ectopic pregnancies may also rarely occur in the rudimentary horn. Such ectopic pregnancies can lead to massive hemorrhage as they can grow to relatively large size before rupturing. Therefore, if a rudimentary horn is documented, surgical resection is usually recommended. The poorest fetal survival among all müllerian duct anomalies has been reported with the unicornuate uterus. Spontaneous abortion has been reported to occur in 34%, preterm labor in 20%, and intrauterine demise in 10%. The live birth rate is estimated to be only 50%. The unicornuate uterus seems to be the most difficult müllerian duct anomaly to confidently diagnose on sonography because it can be confused and misdiagnosed as a small uterus. Looking for the contralateral rudimentary horn, which can be filled with blood, may sometimes help. The rudimentary horn may have a distended and dystrophic appearance and should not be mistaken for an adnexal mass. MRI is considered the study of choice in resolving these complicated situations. Recently 3D ultrasound has been reported to be useful in diagnosis, allowing visualization on the coronal imaging plane of a single asymmetric endometrial cavity that is laterally deviated, with or without a rudimentary horn. Forty percent of cases are reported to have renal anomalies, typically ipsilateral to the rudimentary horn, most often renal agenesis or pelvic kidney.Complete failure of fusion of the müllerian ducts leads to development of two separate uteri, each with its own cervix, termed uterus didelphys (Fig. 28-13). This didelphys is a relatively rare anomaly accounting for fewer than 5% of all müllerian duct anomalies. The endometrial cavities of each hemiuterus do not communicate. A longitudinal or oblique vaginal septum is common, but not always present. An oblique septum may be obstructive and such patients will present with hematocolpos, dysmenorrhea, pelvic mass, vaginal discharge, or pelvic pain. The vaginal septum may also lead to dyspareunia and even rarely vaginal dystocia during vaginal delivery. If no obstruction is present, most patients are asymptomatic and uterus didelphys is an incidental finding. Patients with uterus didelphys usually successfully carry pregnancies to term,and infertility is an uncommon presentation. On ultrasound images, the two widely separated
fundal horns with a deep fundal cleft, two uterine cavities, and two separate cervices can be identified. However, the vaginal septum is better evaluated on physical examination and with MRI or CT (Fig. 28-14), although occasionally 3D US imaging may be helpful. Unilateral renal agenesis is often present, particularly in the setting of obstructed uterus didelphys.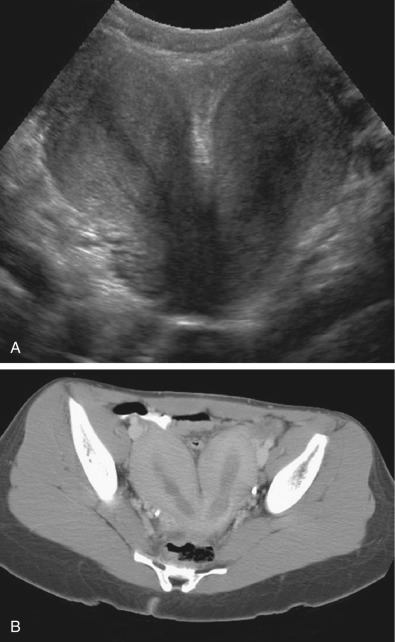 FIG 28-14 A, Coronal transvaginal view of a didelphys uterus with completely separate right and left cavities and deep intervening cleft between the two horns. B, Axial computed tomography scan of the same patient demonstrating a uterine didelphys with widely splayed uterine horns. A rare syndrome that can be seen in the setting of uterus didelphys is obstructed hemivagina ,and ipsilateral renal anomaly (OHVIRA); some cases do not fit the classic definition. An absent kidney in the expected anatomic location should trigger a search for an ectopic or possibly a dysplastic/atrophic kidney. If obstructed hemivagina is seen, this finding should also trigger a search for possible ectopic insertion of a ureter. Obstructed hemivagina and ipsilateral renal agenesis syndrome should be redefined as ipsilateral renal anomalies: cases of symptomatic atrophic and dysplastic kidney with ectopic ureter to obstructed hemivagina.Partial fusion of the two müllerian ducts with incomplete fusion at the fundus leads to formation of a bicornuate uterus and a single cervix (Fig. 28-13). The bicornuate uterus is estimated to account for approximately 10% of all müllerian duct anomalies. The fundal contour of the bicornuate uterus is concave, and the two horns are divergent. MRI criteria based on this appearance are an *intercornual distance greater than 4 cm and a *fundal cleft depth 1 cm or more between the horns. Patients with bicornuate uterus have few reported obstetric problems, and most cases are discovered incidentally. However, an increased incidence of cervical incompetence has been reported. Decreased size of the uterine cavity has also been reported to be associated with poor fetal outcome. Sonographically, in a bicornuate uterus, the endometrial cavities are widely separated, and a deep indentation in the fundal contour is obvious. Imaging of the fundal contour requires obtaining an image in a coronal plane, which is often easiest with transabdominal pelvic US if the uterus is anteverted and anteflexed or with 3D transvaginal imaging. MRI is often recommended for definitive diagnosis. The bicornuate uterus should be distinguished from a uterine didelphys, and a single cervix should be documented to confirm the diagnosis of a bicornuate uterus (Fig. 28-15). However, if two endocervical canals are present, such as in the bicornuate bicollis uterus, identification of a vaginal septum can be the only way to discriminate between a bicornuate bicollis and didelphys uterus. Unfortunately, one fourth of bicornuate uterus cases have been reported to have a vaginal septum as well, which makes them indistinguishable from didelphys. MRI is the optimal imaging technique for evaluation of vaginal septa. Often in these complex cases with overlapping appearances, it is best to describe what is seen on MRI rather than to attempt to categorize.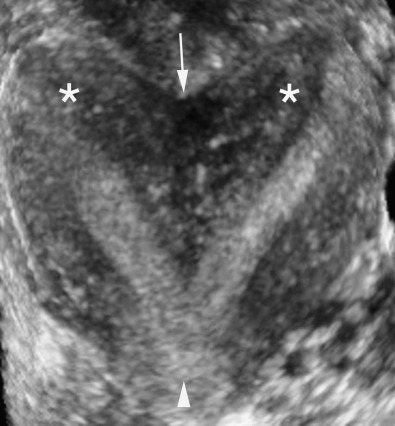 FIG 28-15 A coronal three-dimensional image demonstrating a heart-shaped bicornuate uterus. Fundal indentation is well seen ( arrow ), as well as the widely divergent horns ( asterisks ) with a single cervix and endocervical canal ( arrowhead )Failure of resorption A/ of the septum after complete fusion of the müllerian ducts leads to formation of a septate uterus (Fig. 28-13), B/ which is the most common type of müllerian duct anomaly, C/ accounting for close to 55%. D/ The fundal contour between the two endometrial cavities is convex, flat, OR or indented less than 1 cm. The septum may be E/ partial (if partial resorption has occurred) or complete, extending to the internal cervical os and sometimes through the cervix to the external os. F/ The septum can contain fibrous or myometrial tissue. G/ The endometrial cavities are typically symmetric. Many women with a septate uterus, H/ experience repeated miscarriages, usually in the first trimester, with a reported incidence of miscarriage of 65% and an incidence of premature birth of nearly 20%. Confirming this type of anomaly is clinically important because I/ metroplasty is reported to improve fetal survival. Metroplasty may be performed hysteroscopically in women with a septate uterus, whereas surgical J/ repair/resection in a patient with a bicornuate uterus must be performed transabdominally, although surgical correction is less often required. On sonography, *the smooth fundal contour (either convex, flat, or indented <1 cm) is diagnostic, but requires obtaining an image of the fundus in the coronal plane, which can be difficult on transvaginal imaging and is more easily accomplished with 3D imaging or occasionally with transabdominal imaging if the uterus is anteverted and anteflexed. *There is less divergence between the two endometrial cavities, which are usually separated by a very thin septum (Fig. 28-16). *The septum can extend all the way to the external os or even upper vagina. If the septum does not extend to the internal cervical os, it should be described as a partial septate uterus. Because of superior multiplanar imaging capability, MRI is generally considered the most definitive imaging modality for distinguishing a septate from a bicornuate uterus as obtaining a true coronal image through the uterine fundus is routinely possible on MRI. K/ It is the depth of the fundal notch between
the two uterine horns that is the primary diagnostic criterion rather than the composition of the septum
Evaluation of associated renal anomalies and for the presence of a vaginal septum is also easily accomplished with MRI. However, advances in the use of 3D ultrasound have made it possible to visualize the fundal contour in many patients, and 3D sonography is replacing MRI in some centers for at least initial evaluation of uterine congenital anomalies.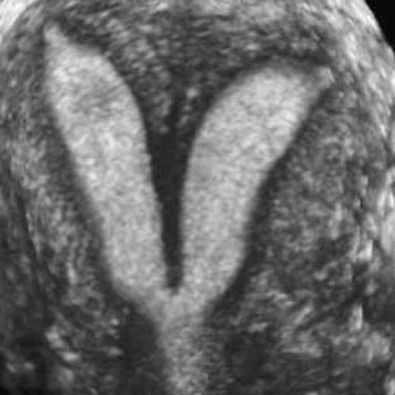 https://radiologykey.com/ultrasound-evaluation-of-the-uterus-2/ https://radiologykey.com/ultrasound-evaluation-of-the-uterus-2/
| |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: Obstetric US Imaging and the Obese Patient موضوع: Obstetric US Imaging and the Obese Patient  الخميس أغسطس 01, 2024 6:50 pm الخميس أغسطس 01, 2024 6:50 pm | |
| Obstetric Ultrasound Imaging and the Obese Patient Summary of Key PointsObesity is epidemic and a significant public health problem.
Obese women are at increased risk of maternal complications of pregnancy compared to
women of normal weight.
Fetuses of obese gravidas are at increased risk of malformations compared to those of
normal weight women.
Ultrasound imaging of obese patients is hampered by acoustic noise, artifacts, and thicker
anterior abdominal wall, all of which degrade the image.
Over 60% of the population of the United States is considered overweight, and more than one third is obese, making obesity a significant public health problem. In 2005, the World Health Organization estimated that 1.6 billion adults worldwide were overweight and 400 million were frankly obese (body mass index [BMI] ≥ 30). This worldwide epidemic shows no sign of abating (decreasing or subsiding) and continues to increase, especially in the United States. A growing body of evidence shows that obese patients have a higher risk of a multitude of health problems, including heart disease, type 2 diabetes, hypertension, stroke, “metabolic syndrome,” arthritis, cancer, respiratory problems, sleep apnea, pregnancy complications, and more (Table 25-1). The National Institutes of Health and the World Health Organization define obesity according to the BMI (in kg/m 2 ). A BMI of 18 to 24.9 is normal, and a BMI of 25 to 29.9 is overweight. Classes I, II, and III obesity are defined as BMIs of 30 to 34.9, 35 to 39.9, and 40 or higher, respectively. TABLE 25-1 Risks Associated With Maternal Obesity [th]Maternal Risks [/th][th]Fetal Risks [/th] | Cardiovascular disease | Congenital anomalies | | Hypertension | Lower detection of fetal anomalies | | Recurrent miscarriage | Macrosomia | | Gestational diabetes | Inaccurate fetal weight estimate | | Preeclampsia | Preterm birth | | Cesarean delivery | Stillbirth and neonatal death | | Postpartum hemorrhage |
| | Wound infection |
| | Thromboembolism |
| | Maternal death |
|
Obese women have an increased risk for adverse pregnancy outcomes that impact both
the mother & the fetus. Table 25-1 lists the most common maternal and fetal complications
associated with maternal obesity. In addition, an increased risk of fetal malformations has
been associated with obesity, and fetal anomalies such as neural tube defects, cardiac anomalies, anal atresia, and limb reduction abnormalities are reported to be significantly more common with obese patients compared to the normal weight population ( Table 25-2 ). TABLE 25-2 Fetal Anomalies Associated With Maternal Obesity [th]Anomaly [/th][th]OR (95% CI) [/th] | Anal atresia | 1.48 (1.12-1.97) | | Cardiac defects | 1.30 (1.12-1.51) | | Hydrocephalus | 1.68 (1.19-2.36) | | Limb reduction | 1.34 (1.03-1.73) | | Neural tube defect | 1.87 (1.62-2.15) |
CI, confidence interval; OR, odds ratio.
Obese gravidas require more medical resources than normal weight patients and often present difficult technical problems for the medical personnel providing their care. High BMI patients have been reported to require more interventions and care of all types, including obstetric ultrasound examinations, medications, telephone calls to providers, and prenatal visits with physicians compared to women of normal weight. In addition to requiring more numerous ultrasound examinations, the examinations required to detect fetal anomalies and pregnancy complications are often more technically challenging in obese compared to thinner patients. The quality of the ultrasound examination done on an obese patient is technically inferior when compared to the same scan done on slimmer patients owing to the distance traversed by the sound beam and the density of adipose tissue. Hence, the quality of the US image relates inversely to the distance that the beam must travel to reach the fetus. The US beam is absorbed, dispersed, and attenuated in adipose tissue, limiting the image quality in evaluation of the fetus. The US image is further degraded with each centimeter that it penetrates through the body to reach the fetus. As a result, the most obese patients who are at the highest risk of maternal and fetal complications also have the poorest quality imaging by US. Over time, advances in US technology have resulted in improved image quality even in the more challenging patients. Preprocessing and postprocessing filters, speckle-reduction filters, compound imaging, and tissue harmonic imaging have all contributed to improved image quality. Despite these new tools, the US image in obese gravidas often remains fuzzy and noisy and suffers from excessive backscatter and artifacts ( Fig. 25-1 ). 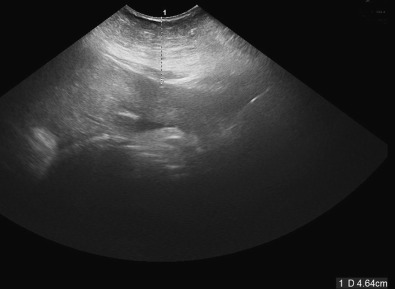 FIG 25-1 This is an attempt at imaging a third trimester fetus in an obese patient. Note the very echogenic adipose tissue in the anterior abdominal wall that attenuates the sound before it reaches the fetus. https://radiologykey.com/obstetric-ultrasound-imaging-and-the-obese-patient/ | |
|   | | | | UTERUS & OVARIES |  |
|
مواضيع مماثلة |  |
|
| | صلاحيات هذا المنتدى: | لاتستطيع الرد على المواضيع في هذا المنتدى
| |
| |
| |
|


