
موقع د. كمال سيد الدراوي
طبي_ اكاديمي _ ثقافي _ تعليمي _ _ استشارات طبية_فيديو طبي
|
|
| | كل يوم معلومه أساسيه |  |
| | |
| كاتب الموضوع | رسالة |
|---|
د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: رد: كل يوم معلومه أساسيه موضوع: رد: كل يوم معلومه أساسيه  الجمعة نوفمبر 03, 2023 7:22 pm الجمعة نوفمبر 03, 2023 7:22 pm | |
| Can a blood test confirm miscarriage?
Blood tests.
A low or falling level of hCG could be a sign of pregnancy loss. If the pattern of changes in your hCG level is irregular, your health care professional may recommend more blood tests or an ultrasound. Your blood type also might be checked
What color discharge is a miscarriage?
The most common sign of miscarriage is vaginal bleeding.
This can vary from light spotting or brownish discharge to heavy bleeding and bright-red blood or clots. The bleeding may come and go over several days
What week is the highest risk of miscarriage?
Risk rates
Weeks 0 to 6. These early weeks mark the highest risk of miscarriage. ...
Weeks 6 to 12. Once a pregnancy makes it to 6 weeks and has confirmed viability with a heartbeat, the risk of having a miscarriage drops to 10 percent . ..
Weeks 13 to 20. By week 12, the risk may fall to 5 percent
Can duphaston prevent miscarriage?
This medication is designed to help maintain the pregnancy until the placenta has formed. Duphaston is used during pregnancy: to minimise the risk of miscarriage. If the pregnant woman is diagnosed
with uterine contractions that can lead to preterm labour.
Can I take progesterone after a miscarriage?
If someone who has had a previous miscarriage starts bleeding, they should now be treated with progesterone as this slightly reduces the chance of miscarriage. The guideline says progesterone should be given if the pregnancy is in the womb, and potentially normal, until 16 weeks of pregnancy.
What not to do after miscarriage?
No sex, tampons, or douching for 2 weeks.
Wait at least 1 normal period before you try to get pregnancy.Oct 19, 202
What are the disadvantages of D&C ?
D&C (Dilatation & Curettage) risks include:
Uterine perforation (a small tear in your uterus), which may happen if the tip of the curette passes through your uterine wall.
Uterine infection.
Uterine bleeding. | |
|   | | د.كمال سيد
Admin




عدد المساهمات : 2690
نقاط : 4494
السٌّمعَة : 9
الجنس : 
علم بلدك : 
تاريخ الميلاد : 03/04/1950
تاريخ التسجيل : 30/07/2012
العمر : 74
الموقع : السودان - سنار
العمل/الترفيه : طبيب عمومى وموجات صوتية
الساعة الان :
دعائي : 
 |  موضوع: US Evaluation of the Uterus موضوع: US Evaluation of the Uterus  الأربعاء يوليو 31, 2024 12:02 pm الأربعاء يوليو 31, 2024 12:02 pm | |
| US Evaluation of the Uterus contd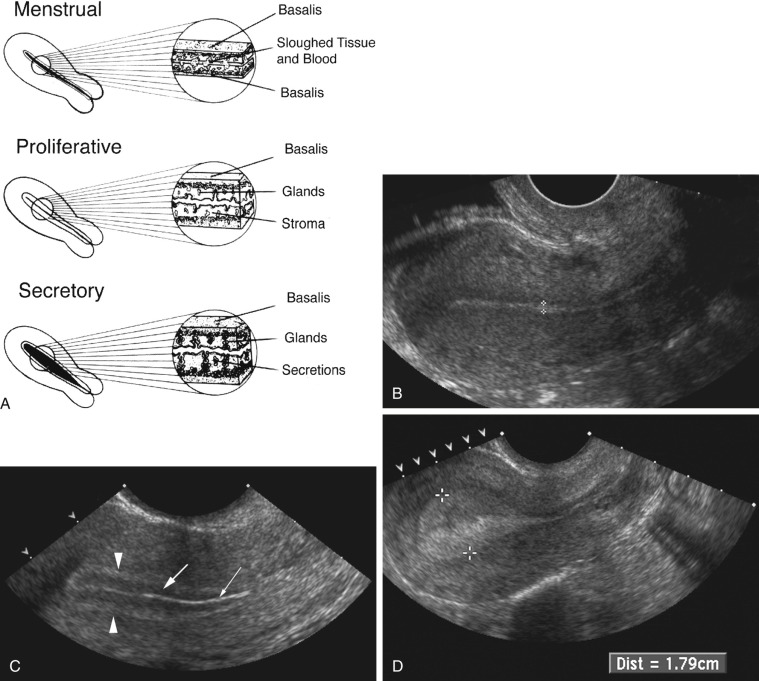 FIG 28-3 A, Diagram depicting normal development of the endometrium during the menstrual, proliferative, and secretory phases. In the menstrual phase, the endometrium appears as a A/ thin, B/ irregular interface. The C/ central echogenicity probably arises from sloughed tissue and blood. In the proliferative phase, the endometrium A/ is relatively hypoechoic, likely a B/ reflection of the straight and orderly arrangement of the glandular elements. C/ The central thin, echogenic line is likely a specular reflection from the endometrial surfaces. In the secretory phase, the endometrium achieves its A/ maximum thickness and B/ echogenicity. This appearance is from the distended and tortuous glands, which contain secretions. FIG 28-3 A, Diagram depicting normal development of the endometrium during the menstrual, proliferative, and secretory phases. In the menstrual phase, the endometrium appears as a A/ thin, B/ irregular interface. The C/ central echogenicity probably arises from sloughed tissue and blood. In the proliferative phase, the endometrium A/ is relatively hypoechoic, likely a B/ reflection of the straight and orderly arrangement of the glandular elements. C/ The central thin, echogenic line is likely a specular reflection from the endometrial surfaces. In the secretory phase, the endometrium achieves its A/ maximum thickness and B/ echogenicity. This appearance is from the distended and tortuous glands, which contain secretions.
B, Postmenstrual transvaginal sagittal image of the uterus demonstrating the normal thin homogeneously echogenic early proliferative endometrium (calipers).
C, Transvaginal sagittal image of the periovulatory endometrium. A/ A three-layered endometrium is seen, giving the endometrium a B/ striated appearance: the collapsed endometrial lumen is demonstrated by the very thin central echogenic line (thin arrow). The A/ surrounding B/ hypoechoic layer representing the edematous functionalis endometrium (thick arrow). and an outer hyperechoic layer representing the basal endometrium (arrowheads) are seen. D, Transvaginal sagittal image of the secretory endometrium. In the secretory stage of the menstrual cycle, the endometrium (calipers) becomes A/thick and B/more homogeneouslyC/ echogenic.
SIS, (Saline Infusion Sonogram) or as it is often referred to, sonohysterography, is an innovative technique used to evaluate a variety of endometrial and myometrial processes that involve the endometrial canal. The most common indications for SIS include, but are not limited to, evaluation of the following:
Abnormal uterine bleeding
Uterine cavity, especially with regard to uterine leiomyomas, polyps, and synechiae
Abnormalities detected on transvaginal sonography, including focal or diffuse endometrial or intracavitary abnormalities
Congenital abnormalities of the uterus
Infertility
Recurrent pregnancy loss
SIS is contraindicated in women who could be pregnant or have an active infection. Because the normal secretory endometrium may be thick and simulate endometrial disease, the examination should be scheduled in premenopausal women during the follicular phase of the menstrual cycle, after menstrual flow has ceased but prior to ovulation, no later than the 10th day of the menstrual cycle. Active vaginal bleeding is not generally a contraindication but can make imaging challenging or even nondiagnostic. At our institution, we perform a preliminary transabdominal and transvaginal sonogram before SIS. After the procedure is explained to the patient, the external os is cleansed before catheterization of the cervical canal using aseptic technique. A sonohysterography catheter (flushed with saline to remove any air bubbles) is then advanced into the endometrial canal. Once in the endometrial canal, the balloon is inflated (preferably with saline rather than air to avoid shadowing) so that the catheter does not become dislodged. However, some clinicians prefer to use a catheter without a balloon. The speculum is removed, and the transvaginal probe is reinserted adjacent to the catheter. Under ultrasound guidance, the balloon is gently retracted to occlude the internal os. Sterile saline should be administered under real-time sonography. The amount of saline introduced is variable, often between 5 and 30 mL. Normal anatomy and abnormal findings should be documented in two separate imaging planes using a high-frequency transvaginal probe, and the endometrium should be fully evaluated from one cornua to the other ( Fig. 28-4 ). Additional techniques such as color Doppler and 3D imaging may be helpful in evaluating both normal and abnormal findings. 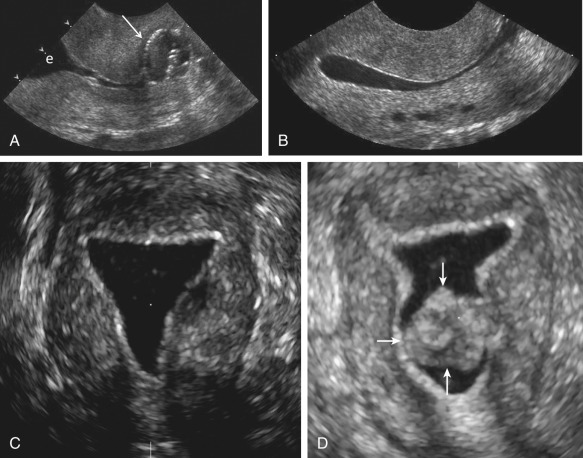 FIG 28-4 Saline-infused sonohysterogram. A, Transvaginal sagittal image of the cervix demonstrating the catheter balloon ( arrow ) positioned in the lower endocervical canal. Anechoic fluid is in the upper endocervical canal and lower endometrial cavity (e). B, Transvaginal sagittal image after saline infusion. The normal thin echogenic endometrium is well seen circumferentially. The endometrial cavity is filled with anechoic fluid. Note several small, round anechoic structures in a linear configuration in the posterior wall of the myometrium. These are the arcuate vessels and would fill in with color Doppler. C, A coronal three-dimensional reconstruction after saline infusion, demonstrating the normal regular, thin, echogenic endometrium without any intracavitary abnormalities. D, In comparison, a coronal three-dimensional reconstruction after saline infusion revealed a 100% intracavitary leiomyoma ( arrows ), separate from the thin, regular echogenic endometriuhttps://radiologykey.com/ultrasound-evaluation-of-the-uterus-2/m. FIG 28-4 Saline-infused sonohysterogram. A, Transvaginal sagittal image of the cervix demonstrating the catheter balloon ( arrow ) positioned in the lower endocervical canal. Anechoic fluid is in the upper endocervical canal and lower endometrial cavity (e). B, Transvaginal sagittal image after saline infusion. The normal thin echogenic endometrium is well seen circumferentially. The endometrial cavity is filled with anechoic fluid. Note several small, round anechoic structures in a linear configuration in the posterior wall of the myometrium. These are the arcuate vessels and would fill in with color Doppler. C, A coronal three-dimensional reconstruction after saline infusion, demonstrating the normal regular, thin, echogenic endometrium without any intracavitary abnormalities. D, In comparison, a coronal three-dimensional reconstruction after saline infusion revealed a 100% intracavitary leiomyoma ( arrows ), separate from the thin, regular echogenic endometriuhttps://radiologykey.com/ultrasound-evaluation-of-the-uterus-2/m. | |
|   | | | | كل يوم معلومه أساسيه |  |
|
مواضيع مماثلة |  |
|
| | صلاحيات هذا المنتدى: | لاتستطيع الرد على المواضيع في هذا المنتدى
| |
| |
| |
|


