Ultrasound of hemodialysis accessUltrasound has an important role in planning temporary and permanent hemodialysis access, for
examining permanent access fistulas and grafts prior to first use, and in the investigation of complications in these fistulas and grafts. Ultrasound may be used for
routine monitoring of access flow, although other methods are also available.
Portable ultrasound scanners may be used in dialysis units to aid needling where access is difficult. For a more detailed examination of the access, radiology departments and vascular laboratories are equipped to undertake ultrasound investigation of the
whole access circuit. The high flows, unusual hemodynamics, and anatomy of fistulas and grafts can make this a challenging investigation but it is potentially a rewarding one. Ultrasound is a quick, safe, and effective means to identify existing and impending problems, enabling early radiological or surgical intervention to prolong the use of the existing access and to plan effective alternatives.
HEMODIALYSIS ACCESSHemodialysis requires high blood flow, from
250 to 400 ml/min, to the extracorporeal dialyzer. Hemodialysis is used in both acute and chronic renal failure.
Acute renal failure
Following a sudden loss of renal function,
1/ dialysis is usually via a c
entral venous catheter. Ultrasound is used to
2/ examine
central, neck, and arm veins and to
3/ guide catheter placement. In patients with reversible failure, dialysis is discontinued as the kidneys recover. In kidneys with
4/ irreversible failure,
permanent access is planned, since central venous catheters have a limited life.
Chronic renal failure
Once chronic end-stage renal failure is identified,
1/ measurement of the patient’s creatinine levels and estimated glomerular filtration rate (eGFR) are used to
determine the impending need for dialysis. Ideally, as the prospect of dialysis approaches, permanent access is planned and surgery undertaken so that the access is ready in time for first use.
Permanent
2/ access, through a fistula or graft,
requires high flows through a superficial vein or graft that can be repeatedly needled (
Fig. 16.1), is easy to keep clean, and is comfortable for the patient during periods of dialysis –
typically 4 hours three times a week. American and European reviews and guidelines have been produced and are regularly updated to foster good hemodialysis practice (
National Kidney Foundation 2006;
Tordoir et al. 2007). Both contain comprehensive bibliographies. Amongst challenges for the clinical teams that may involve ultrasound investigation are the need to increase the number of patients with a permanent access in place when they first present for dialysis, identifying the most appropriate access site for patients, and maintaining effective surveillance to reduce the incidence of complications and access failure.
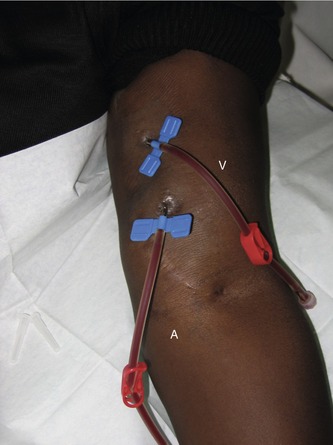
Figure 16.1 Needles inserted into the basilic vein of a brachial artery/transposed basilic vein fistula prior to dialysis. The distal, upstream, needle is referred to as the arterial needle (A) from which blood is drawn for dialysis. Blood is returned through the venous needle (V).
Access sites
Permanent hemodialysis accesses can be either an
arteriovenous fistula where the vein is used for needle access or a prosthetic graft between an artery and vein.
Fistulas generally have a
lower incidence of complications than grafts (0.2 events/patient per year versus 0.8–1.0 events/patient per year for European Best Practice Guidelines) and
superior long-term patency. Grafts can be used earlier following surgery whereas fistulas need more time for the vein to develop and diameter to increase, typically 6 weeks postoperatively.
Recommendations are to use fistulas where possible initially.
An
AV fistula is
a connection that's made between an artery and a vein for dialysis access. A surgical procedure, done in the operating room, is required to
stitch together two vessels to create an AV fistulaThere are several possible sites for fistulas and grafts in the arms. Once arm accesses are exhausted, femoral artery to femoral vein grafts may be used. Several unusual variations of grafts and veins are possible where access is difficult, depending on the preference of the surgeon and the availability and access of suitable arteries and veins.
These fistulae are typically fashioned to connect
the radial artery to the cephalic vein, the brachial artery to the cephalic vein, or the brachial artery to a basilic vein.
A surgeon usually performs the procedure in the operating room. You receive a
local anesthetic (numbing medicine) at the proposed site along with
IV sedation to relax you. Discomfort is minimal and you may even fall asleep during the
1 to 2 hour-long procedure.
An AV fistula is
the best means of access to the blood stream for long-term haemodialysis. It means that there is
no plastic dialysis line to become infected. This is particularly important as infections damage the lining of the blood vessel and cause it to become narrow.
hat are the rules of 6 AVF?
The Rules of 6 (
flow volume >600 mL/min, vein diameter >6 mm, vein depth <6 mm) are widely used to determine when an arteriovenous fistula (AVF) will support dialysis.Feb .
disadvantages of AV fistulaAV fistulas
may not be suitable for people with small or weak veins. – The most common problem with the AV fistula is stenosis, the narrowing of the blood vessel, which may lead to a decrease in blood flow or
formation of blood clots. – Strengthening the AV fistula requires daily exercises
- Do not let anyone draw blood or put an IV in your access arm. ...
- Do not have your blood pressure taken in your access arm.
- Do not wear a tight sleeve, a watch, or other constricting jewelry on your access arm.
- An AVF can occur anywhere in the body, though we mostly find them in the head, neck, spine, and liver. The connection between a high-pressure artery and a low-pressure vein can increase the blood flow through the area, which often expands both the artery and the vein.
- Rule of 7 in dialysis
- An informal algorithm that has been commonly advocated for decades is the “rule of seven”, in which the pre-dialysis serum potassium level is subtracted from seven to determine the dialysate
- potassium that should be assigned
- Data in the literature on DUS flow volume assessment indicate that a well-functioning AVF will be characterized by a flow rate of 700–1,300 ml/min
The main sites for fistulas and grafts are listed in
Box 16.1 and shown diagrammatically in
Figure 16.2. The nondominant arm is generally used initially.
Box 16.1 shows an approximate order of preference; the choice for an individual patient depends on many factors. For example, a young patient with good peripheral arm vessels may be a better candidate for a radiocephalic fistula whereas an elderly patient with diabetes and known peripheral vascular disease might start dialysis with a more proximal access. A major advantage of a peripheral fistula is that it may leave more proximal vessels available for future access
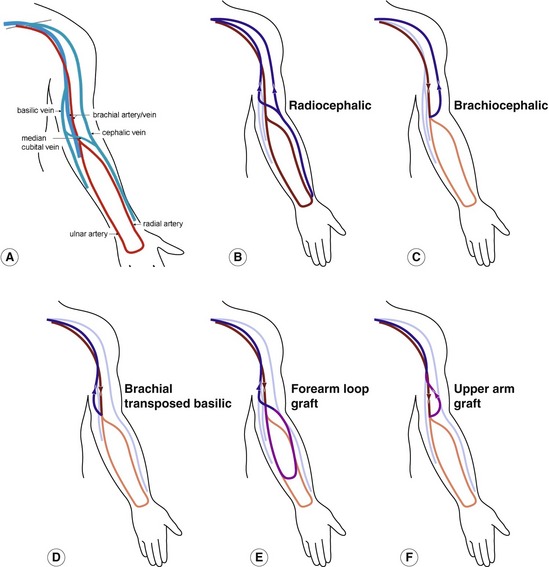
Figure 16.2 Diagram of common arm fistula and graft sites. (A) Main arm vessels. In the other images, the arterial supply and venous drainage for the high-flow dialysis access circulation are shown in bold. (B) Radiocephalic. (C) Brachiocephalic. (D) Brachial transposed basilic. (E) Forearm loop graft. (F) Upper-arm graft.
Temporary access – role of ultrasound
Ultrasound is useful to assess central veins to ensure patency for emergency central dialysis catheter placement in patients with acute renal failure or failed permanent access. The patient should be lying flat so that the central veins are not collapsed. The internal and external jugular veins are examined using a low-frequency (4–8 MHz) linear array in B-mode and with color and pulsed Doppler to ensure patency and normal venous flow patterns. The subclavian veins may be imaged in long section either supraclavicularly or infraclavicularly (
Fig. 16.3). The subclavian vein often collapses during the cardiac cycle or in response to breathing. The right and left proximal internal jugular vein and subclavian veins may be difficult to image with a linear array due to clavicle, sternum, and ribs which restrict ultrasound access. A small footprint phased or tightly curved array (
Fig. 16.4) aids in color flow imaging of these veins (
Fig. 16.5) and the brachiocephalic veins, although B-mode images are poor and compression of all these veins, to rule out deep-vein thrombosis, is impossible.
https://radiologykey.com/ultrasound-of-hemodialysis-access/next


